Diabetologia:患有1型糖尿病的儿童表现出血浆蛋白和IgG的N-糖基化改变
2022-06-06 从医路漫漫 MedSci原创
血浆蛋白的N-糖基化是一个严格调节的非常复杂的酶促过程,通过该过程不同的寡糖被添加到蛋白骨架上,在许多情况下调节蛋白功能。不要将糖基化与糖化混淆,糖化是一种非酶促反应,如HbA1c。
背景:1型糖尿病是一种病因不明的慢性自身免疫性疾病,以产生胰岛素的胰腺β细胞的破坏为标志。诊断患有1型糖尿病的儿童和青少年人数以每年约3%的速度增长。虽然胰岛自身抗体的测量可以在临床诊断前数年暴露疾病,但连续监测费用昂贵,对幼儿很困难,对成人不够敏感或特异。由于1型糖尿病的早期识别可以最大限度地降低发病率并促进预防,因此开发风险评估工具是一项重要任务。最近建立的遗传风险评分显示了很好的区分值,但是识别有助于风险评估的其他生物标志物将具有很大的价值。血浆蛋白的N-糖基化是一个严格调节的非常复杂的酶促过程,通过该过程不同的寡糖被添加到蛋白骨架上,在许多情况下调节蛋白功能。不要将糖基化与糖化混淆,糖化是一种非酶促反应,如HbA1c。详细的遗传学研究已经确定了在调节添加的聚糖类型中起重要作用的基因,并且还表明N-糖基化基序侧翼的残基影响添加的聚糖类型。人血浆N-糖组在生理条件下在个体中非常稳定,但对各种病理过程非常敏感,因此可以考虑将N-聚糖作为诊断和预后标志物。糖尿病分类可能很困难,因为它取决于诊断时的条件;例如,一些被诊断患有2型糖尿病的个体有胰岛自身抗体。我们之前表明,根据N-聚糖谱,可以区分糖尿病类型,甚至可以识别未来患2型糖尿病病风险增加的个体。与抗体检测相比,成本较低。
在真核生物蛋白质N-糖基化过程中,14种糖被共翻译转移到内质网中的特定天冬酰胺残基,然后在高尔基复合体中被修饰。这导致许多修饰,如分支、岩藻糖基化、唾液酸化等。在生理条件下,约3%的葡萄糖用于氨基己糖生物合成途径,其中合成了N-糖基化过程的供体分子尿苷二磷酸-N-乙酰氨基葡萄糖(UDP-GL cnac)。定义聚糖复杂性(双天线聚糖、三天线聚糖和四天线聚糖)的聚糖分支程度取决于UDP-GlcNAc的可用性。通过己糖胺生物合成途径的葡萄糖流量增加,导致UDP-GlcNAc和潜在的高度分支聚糖水平升高。我们之前报道了血糖不稳定的成年1型糖尿病患者复杂的高度分支的血清N-聚糖增加。此外,甘露糖结合凝集素的血浆水平在1型糖尿病人群中增加,甘露糖结合凝集素在与特定糖残基结合时激活补体途径之一。T细胞蛋白的异常N-糖基化与1型糖尿病的发病有关。全基因组关联研究确定编码岩藻糖基转移酶2的糖基转移酶基因是1型糖尿病的易感基因之一。
目的:血浆N-糖基化的个体差异主要在糖尿病并发症的背景下进行研究,其在1型糖尿病发病中的作用在很大程度上是未知的。我们的目的是对新近发病的1型糖尿病患者的血浆和IgG N-糖体进行详细描述,并评估它们在风险评估中的鉴别潜力。
方法:在研究的第一部分中,对DanDiabKids注册研究人群的血浆和IgG N-聚糖进行色谱分析,该研究人群包括1917名新诊断为1型糖尿病的儿童和青少年(0.6-19.1岁)。一项后续研究将其中188名参与者的结果与其244名未受影响的兄弟姐妹的结果进行了比较。N-聚糖丰度与各种自身抗体(针对IA-2、GAD、ZnT8R、ZnT8W)的水平和数量的相关性,以及与诊断时的性别和年龄的相关性,通过使用一般线性模型进行评估。使用logistic混合模型弹性网络回归建立疾病预测模型,并使用10倍交叉验证进行评估。
结果:我们的研究表明,1型糖尿病的发病与血浆和IgG高甘露糖比例的增加和GlcNAc结构的二等分,单半乳糖化作用的减少和IgG去唾液酸作用的增加有关。ZnT8R自身抗体水平与二等分GlcNAc的高IgG双半乳糖化聚糖相关。最后,自身抗体数量的增加(比任何单个抗体的水平更能预示糖尿病的进展)伴随着一些高度分支的血浆N-聚糖比例的降低。包括年龄、性别和N-聚糖在内的模型在1型糖尿病儿童和他们的健康同胞之间产生了显著的区分能力,增加血浆和IgG N-聚糖的AUC分别为0.915和0.869。

图1总血浆蛋白(a)和IgG (b)释放的N-聚糖色谱图示例。蓝色方块,N-乙酰氨基葡萄糖(GL cnac);灰色圆圈,甘露糖;黄色圆圈,半乳糖;红色三角形,岩藻糖;紫钻石,N-乙酰神经氨酸(唾液酸)。GP,聚糖峰。
表1直接测量和衍生的血浆N-聚糖与疾病状态的关系,进一步根据年龄和性别进行调整,并根据多重检测进行校正
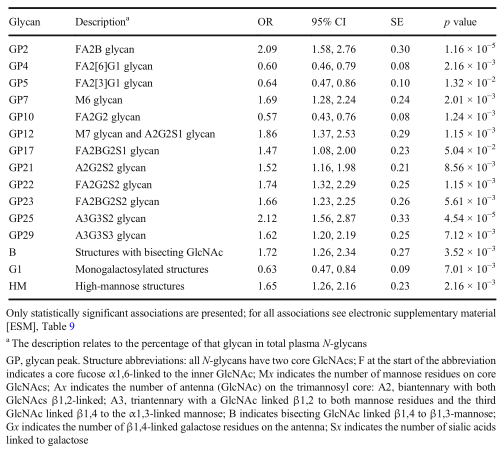
表2直接测量和衍生的IgG N-聚糖与疾病状态的关系,进一步根据年龄和性别进行调整,并根据多重检测进行校正
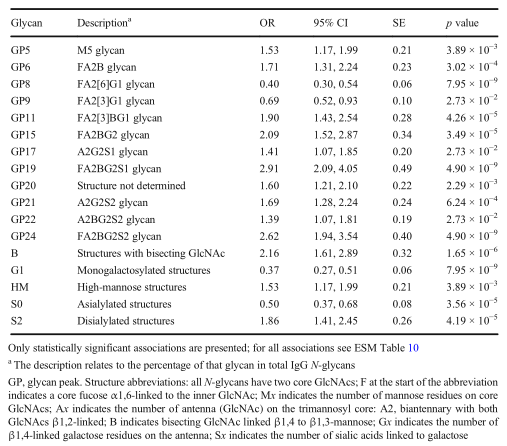
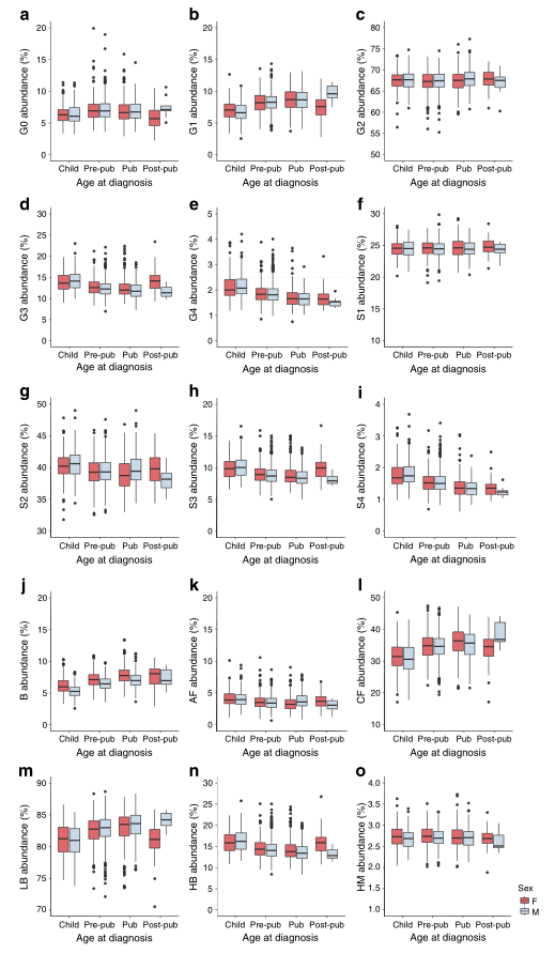
图2在诊断为1型糖尿病时,不同年龄的男性和女性儿童中血浆N-聚糖的比例。儿童,0.6-6岁;Pre-pub,青春期前儿童,6-11/13岁;pub,青春期儿童,11/13-15/16.9岁;Post-pub,青春期后儿童,15/17-19.1/18.3岁;f,女;m,男;G0,无乳糖化聚糖;G1,单半乳糖化聚糖;G2,双半乳糖化聚糖;G3,三半乳糖化聚糖;G4,四半乳糖化聚糖;S1,单唾液酸化聚糖;S2,二水解聚糖;S3,三唾液酸化聚糖;S4,四唾液酸化的聚糖;b、具有二等分GlcNAc的聚糖;AF,具有触角岩藻糖的聚糖;CF,具有核心岩藻糖的聚糖;LB,低支化聚糖;HB,高支化聚糖;HM,高甘露糖聚糖
结论:我们定义了伴随1型糖尿病发作的N-聚糖变化,并开发了一个基于N-聚糖谱的预测模型,该模型可能在风险评估中具有有价值的潜力。对于1型糖尿病预防试验来说,提高检测能力以识别处于疾病发展风险中的个体将是一笔可观的资产。
原文出处:Rudman N, Kifer D, Kaur S, et al.Children at onset of type 1 diabetes show altered N-glycosylation of plasma proteins and IgG.Diabetologia 2022 May 27
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#BET#
46
#DIA#
29
#血浆蛋白#
45
#糖基化#
31
#IgG#
34
好文章,谢谢分享。
52
学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
46