超详细!这4大类祛痰药到底怎么用,一篇文章总结全了!
2022-01-04 图图 MedSci原创
虽然镇咳药常与祛痰剂、平喘药、抗过敏药或镇痛剂合用,但也要避免过多使用祛痰药物,同时应用多种祛痰剂因强烈刺激气道腺体分泌黏液反而使咳嗽加剧。
黏液的分泌和清除对于气道完整性和肺部防御极为重要。正常情况下,黏液在气流和纤毛的作用下从下呼吸道转移到咽部。但当黏液的分泌量或成分改变、纤毛清除功能下降、咳嗽能力不足时,可造成黏液无法有效排出,潴留于气道,与鼻咽、口咽分泌物、细胞碎片和微生物共同形成痰液。
临床常用祛痰方法
包括危险因素干预、物理祛痰以及药物祛痰:
1、危险因素干预:如积极戒烟、减少颗粒物暴露、防治呼吸道感染。吸烟是气道黏液高分泌最常见的危险因素,因此戒烟对于祛痰管理尤为重要。
2、物理祛痰:包括指导患者深呼吸和有效咳嗽、胸背部叩击、体位排痰以及呼气末正压(PEEP)和胸壁高频振荡(HFCWO)等。湿化疗法也是物理祛痰方式的一种,通过湿化气道可降低分泌物黏稠度以促进排出。有报道通过吸入空气中饱和的岩盐气溶胶微粒(直径1~5 μm,浓度3 mg/m3以上),可改善支气管内容物的流变性,从而促进黏液廓清。
3、药物祛痰:给药途径有雾化吸入、口服及静脉滴注。药物雾化吸入除在局部发挥祛痰作用外,同时可湿化气道。
四大类祛痰药物
根据《雾化祛痰临床应用的中国专家共识》(2021年),目前临床常用祛痰药物按照作用机制可分为4类:
恶心性祛痰剂:促进痰液从呼吸道排出的药物,如高渗生理盐水雾化吸入,愈创甘油醚;
黏液溶解剂:即通过裂解黏蛋白复合物间二硫键等方式促进痰液溶解和排出,如N-乙酰半胱氨酸(NAC)和厄多司坦;
黏液调节剂:即通过促进浆液分泌、减少黏蛋白生成等方式调节黏液分泌,主要有氨溴索、溴己新、羧甲司坦等,糖皮质激素和抗胆碱能药物也具有抑制黏液分泌作用;
黏液动力药:即通过促进气道黏膜纤毛运动、改善黏液清除动力学帮助排痰,包括桃金娘油、桉柠蒎、β肾上腺能受体激动剂。此外,一些复方中成药也具有祛痰作用。
常用祛痰药物的特点及用法如下:

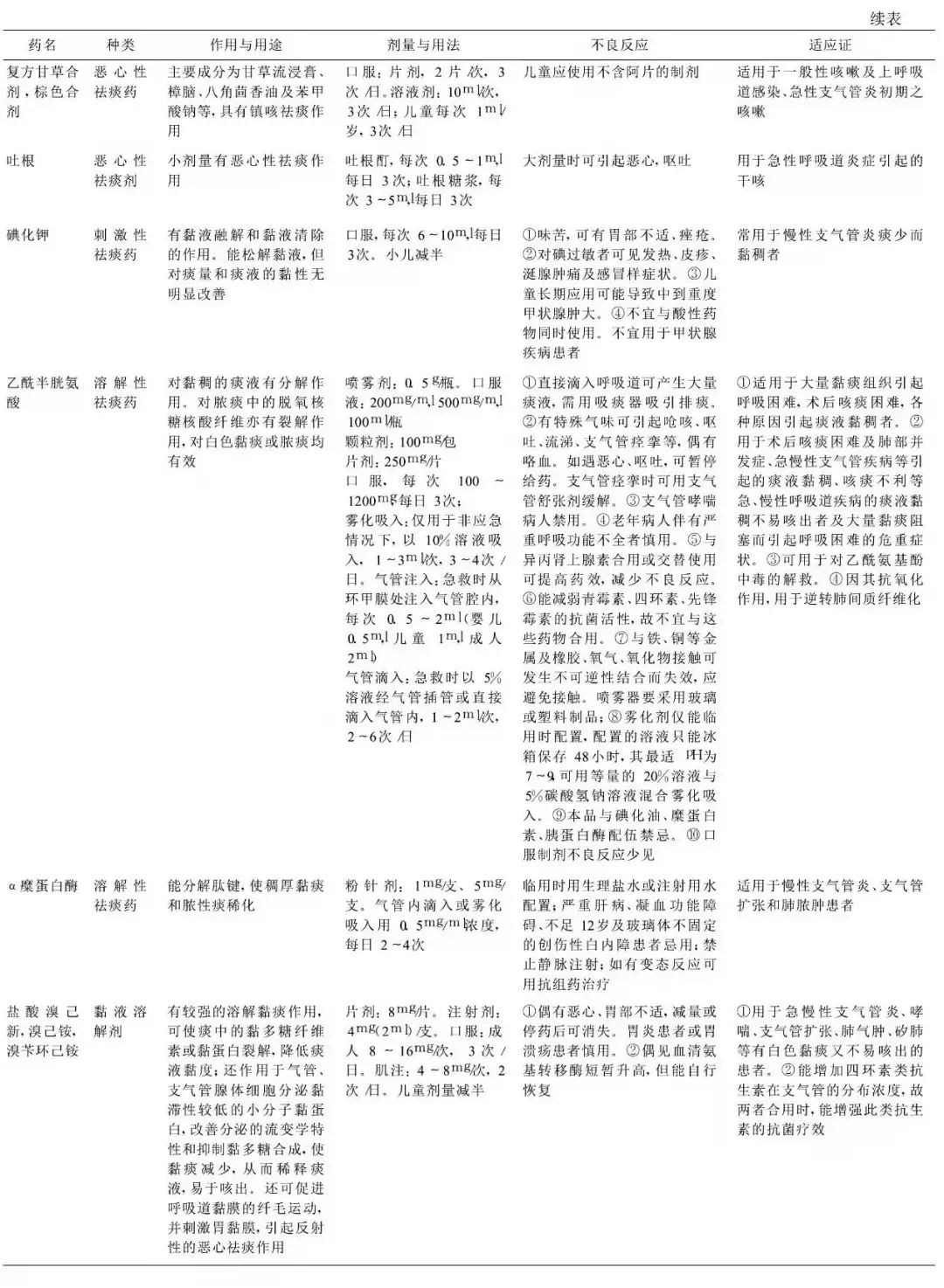
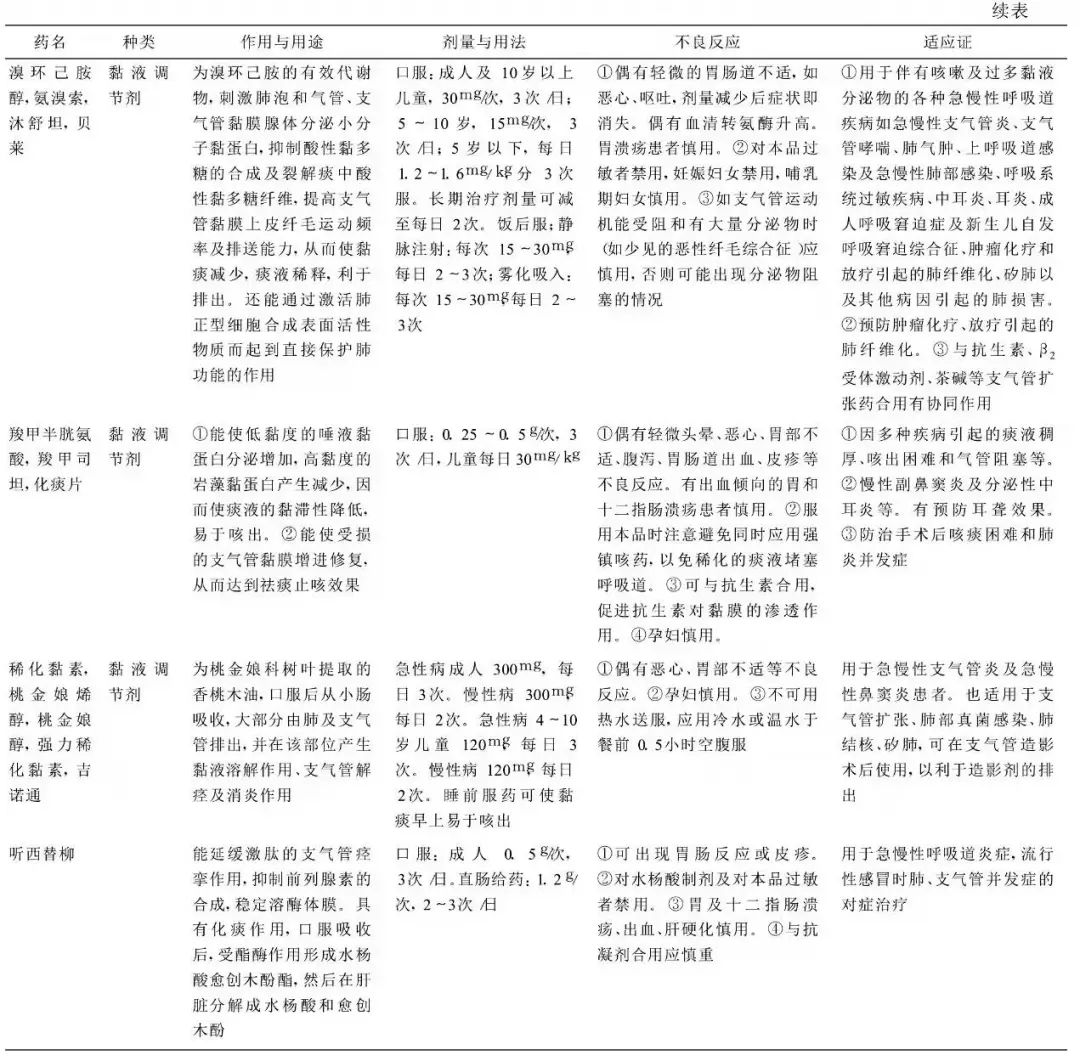
宫巧俐,沈司京.祛痰药物的合理应用[J].中国医刊,2008,(07):59-62.
使用祛痰药物的注意事项:
-
虽然镇咳药常与祛痰剂、平喘药、抗过敏药或镇痛剂合用,但也要避免过多使用祛痰药物,同时应用多种祛痰剂因强烈刺激气道腺体分泌黏液反而使咳嗽加剧。
-
恶心性祛痰药剂量不宜过大以免引起呕吐。因能促使胃酸分泌增加所以对溃疡病患者应慎用。
-
服用氯化铵时应多饮水。
-
当痰量较多时不宜使用镇咳药,尤其是喷托维林、苯丙哌林等此类镇咳药会阻断咳嗽反射导致痰液滞留于气道既影响呼吸又易继发感染故宜先祛痰为主止咳为辅,痰液排出咳嗽自然停止。
-
中草药制剂应根据其药物的辨证合理选择切不可盲目滥用。
参考文献:
1.梁盛华,许志威.镇咳、祛痰药物研究进展[J].中国药房,2015,26(25):3578-3580.
2.宫巧俐,沈司京.祛痰药物的合理应用[J].中国医刊,2008,(07):59-62.
3.任常陵.祛痰药物的分类及其使用方法[J].日本医学介绍,2007(10):468-469.
4.石力夫.祛痰药物知识问答(Ⅰ)[J].药学服务与研究,2011,11(02):161-162.
5.石力夫.祛痰药物知识问答(Ⅱ)[J].药学服务与研究,2011,11(03):241-242.
6. 雾化祛痰临床应用的中国专家共识[J].中华结核和呼吸杂志,2021,44(04):340-348.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习了
52
很有用
42
学习了
48
学习了,有用
53
学习了
52
学习#学习#
42
防治及用药的高度重视,HIV双药单一片剂
37
学习了
29
学习
41
学习了
41