JGH:原发性结直肠癌术后发生第二原发性结直肠癌的危险因素分析
2022-01-27 MedSci原创 MedSci原创
大肠癌是常见的恶性肿瘤,包括结肠癌和直肠癌。大肠癌的发病率从高到低依次为直肠、乙状结肠、盲肠、升结肠、降结肠及横结肠,近年有向近端(右半结肠)发展的趋势。
大肠癌(CRC)是世界上第二大癌症死亡原因,而大肠癌筛查可降低大肠癌死亡率。结肠镜检查是最常见的CRC筛查方法之一,因为它可以直接观察到小的肿瘤性结肠病变。然而,不必要的结肠镜检查可能是相当有害的,因为结肠镜检查的肠道准备工作可能导致脱水或电解质失衡,而且结肠镜检查可能导致结肠穿孔。
因此,关注患CRC的高风险人群是很重要的。一些风险因素已被推荐为CRC筛查的对象,如50岁以上,有CRC阳性家族史,尤其是一级亲属患有CRC的患者。尽管过去的CRC病史也是发展为第二原发性CRC的一个风险因素,但尚未确定何时或如何对第二原发性CRC进行术后监测。本项研究旨在使用风险函数分析来评估发生第二原发性 CRC 或高级别腺瘤 (HGA) 的风险率变化,以便在初次手术后有效识别第二原发性结直肠肿瘤CRC患者。

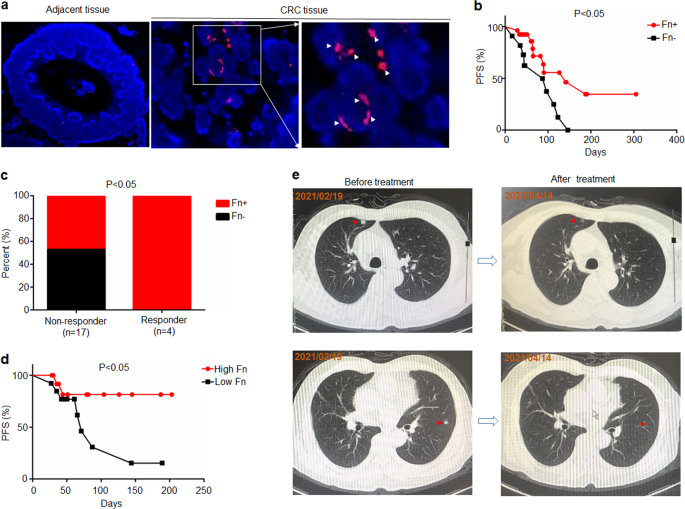
为此,研究人员回顾性招募了 1823 名 0-III 期 CRC 患者,这些患者在 2004 年至 2015 年间接受了根治性手术,并在术后进行了结肠镜检查。研究人员对这些患者进行了随访评估了手术后发生异时性 CRC 和 HGA 的风险率随时间的变化。

研究结果发现继发性结直肠肿瘤的危险函数曲线在术后 1.22 年到一个高峰,该曲线下降至 4年,然后趋于稳定。老年患者的风险高于年轻患者,两者均在1年达到峰值。在年轻患者中观察到另一个峰值出现在术后6和8年。男性患者的风险高于女性患者,有同步病变的患者的风险率明显高于无同步病变的患者,在术后 1 年和 9 年左右有两个明显的发病高峰。

图:直肠癌术后第二原发性肿瘤的发生率
本项研究结果建议所有CRC患者在接受CRC手术后的最初 2 至 3 年内进行强化结肠镜监测,如果患者年龄在 60 岁以下并伴有 CRC 或 HGA,则还建议在术后 6 至 8 年进行更长时间的随访监测。
原始出处:
Kazushige Kawai. Et al. Hazard function analysis for development of second primary colorectal cancer after surgery for primary colorectal cancer. Journal of Gastroenterology and Hepatology.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#原发性#
47
好文章
37
打卡
60
#结直肠#
34