JACC:合并糖尿病的多血管病变患者选择CABG和PCI因人而异
2022-04-17 MedSci原创 MedSci原创
FREEDOM研究后续随访近8年的数据显示,对于合并糖尿病的多血管病变患者,冠状动脉旁路手术(CABG)优于经皮冠状动脉介入治疗(PCI)。
FREEDOM研究后续随访近8年的数据显示,对于合并糖尿病的多血管病变患者,冠状动脉旁路手术(CABG)优于经皮冠状动脉介入治疗(PCI)。
目前,对于这类患者,指南已经明显地倾向于CABG而不是使用药物洗脱支架(DES)进行PCI,但是一直缺乏长期随访的数据,直到这项FREEDOM研究中位随访7.5年的生存数据发表。
值得注意的是,该研究数据显示,与PCI相比,CABG带给65岁以下的患者和曾经吸烟的患者的生存获益尤其显着。CABG和PCI对于65岁以上的老年患者和从不吸烟者的生存获益相似。尽管如此,但个别患者在许多特征上有所不同,会影响治疗的好处和坏处。

FREEDOM评分是在8个患者特征和吸烟-治疗互动的基础上,预测CABG与PCI的不同结果。为了评估5年主要不良心血管事件(MACE)模型在SYNTAX和BEST试验中预测CABG与PCI治疗效益的能力,来自荷兰阿姆斯特丹大学医学中心心脏中心的专家开展了相关研究,结果发表在JACC杂志上。
本研究纳入了702名糖尿病和MVD患者,以反映FREEDOM参与者的情况。通过C-指数评估鉴别力,并通过校准图评估PCI和CABG两组的校准情况。评估了FREEDOM评分预测CABG与PCI治疗效益的能力。
总的来说,与PCI相比,CABG与较低的5年MACE率有关(12.4% vs 20.3%;对数rank P = 0.021),而不考虑吸烟史(Pinteraction = 0.975)。鉴别力和校正力在PCI组都是有帮助的(C-指数=0.69;斜率=0.96,截距=-0.24),但在CABG组是中等的(C-指数=0.61;斜率=0.61;截距=-0.53)。可见,FREEDOM评分显示了治疗效果的一定异质性。
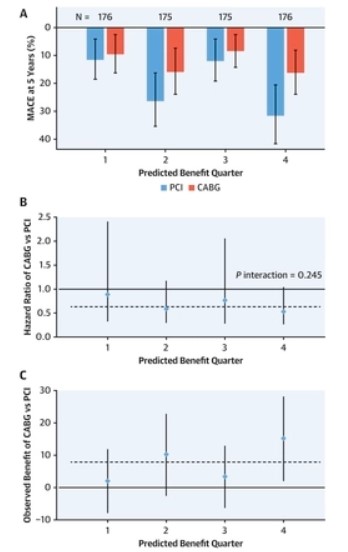
FREEDOM评分可以识别出CABG与PCI的5年MACE的治疗获益的一定异质性。在进行进一步的前瞻性验证之前,在糖尿病和MVD患者中使用FREEDOM评分时应考虑这些结果。
参考文献:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#JACC#
58
#血管病#
59
学习学习了
53
#ACC#
34
#血管病变#
51