一线免疫治疗组合未能改善转移性NSCLC的总体存活率
2018-12-16 MedSci MedSci原创
根据ESMO免疫肿瘤学大会上发表的一项研究显示,使用durvalumab或durvalumab加tremelimumab治疗转移性非小细胞肺癌(NSCLC)的一线疗法并未改善患者的总生存期(OS)。
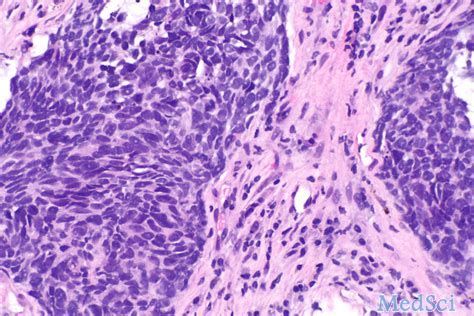
根据ESMO免疫肿瘤学大会上发表的一项研究显示,使用durvalumab或durvalumab加tremelimumab治疗转移性非小细胞肺癌(NSCLC)的一线疗法并未改善患者的总生存期(OS)。开放标签的III期MYSTIC试验(NCT02453282)招募了1,118名没有EGFR致敏突变或ALK重排的患者,并且未接受过转移性NSCLC的先前免疫治疗或化疗。患者随机接受每4周静脉注射durvalumab 20 mg / kg,或durvalumab联合tremelimumab 1 mg / kg静脉注射,每4周一次,共4个周期,或铂类化疗最多6个周期。符合条件的患者允许使用培美曲塞维持治疗。
结果显示,与化疗相比,单独或与tremelimumab一起使用的Durvalumab并未改善OS或无进展生存期(PFS)。哥伦比亚大学医学中心医学博士Naiyer Rizvi报告说:“虽然没有达到统计学意义,但接受durvalumab单药治疗的患者的中位总体生存改善为16.3个月,而PD-L1表达≥25%的患者接受化疗的中位总生存期仅为12.9个月”。在该研究中,488名(44%)具有≥25%或更高的PD-L1表达,40%具有高肿瘤突变负荷(TMB)。
原始出处:
http://www.firstwordpharma.com/node/1611827?tsid=4#axzz5ZoUV0SOC
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#治疗组#
37
#转移性NSCLC#
32
#存活率#
0
#转移性#
32