ERJ:呼吸道症状和肺功能与职业的相关性分析
2022-09-08 小文子 MedSci原创
研究中考虑的职业暴露似乎不是肺功能差异的主要决定因素,尽管它们与更多的呼吸道症状相关。
慢性阻塞性肺疾病与职业暴露有关。European Respiratory Journal杂志在阻塞性肺疾病负担(BOLD)研究中评估呼吸道症状和肺功能与职业暴露的相关性。
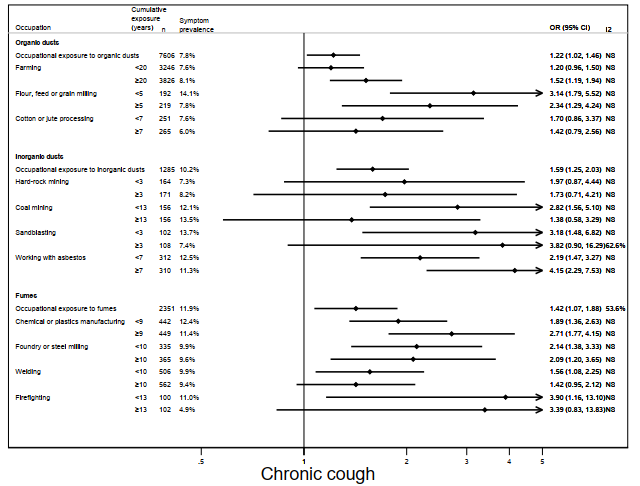
研究人员分析了34个国家28823例成人(≥40岁)的横断面数据。考虑了11种职业,包括耕作,面粉、饲料或谷物研磨,棉花或黄麻加工,硬岩开采,煤矿开采,喷砂,石棉作业,化学或塑料制造,铸造或轧钢,焊接,消防,并按暴露于有机粉尘、无机粉尘和烟雾的可能性进行分组。使用多变量回归评估每个研究地点的慢性咳嗽、慢性咳痰、喘息、呼吸困难、FEV1/FVC和 FVC 与职业的相关性。
结果显示,在粉尘或烟雾暴露较高的环境中工作与呼吸道症状相关,但与肺功能差异无关。最常见的职业是耕作。与未从事任何职业的人相比,从事农民工作≥20年者更易患慢性咳嗽(OR=1.52,95%CI,1.19~1.94)、喘息(OR=1.37,95%CI,1.16~1.63)和呼吸困难(OR=1.83,95%CI,1.53~2.20)。无论暴露持续时间如何,面粉、饲料或谷物研磨与所有呼吸道症状相关。与石棉接触至少7年与慢性咳嗽明显相关(OR = 4.15,95%CI,2.29~7.53)。至少3年的硬岩开采与慢性咳痰有关(OR = 3.91,95%CI,1.79~8.58)。采煤与喘息相关(< 13年;OR = 4.15,95%CI,2.40~7.19)。喷砂与呼吸困难高度相关(< 3年;OR = 4.87,95%CI,2.02~11.76和≥3年;OR = 6.87,95%CI,2.63~17.95)。
男性肺功能的敏感性分析表明,从事有机粉尘暴露工作至少20年与FEV1/FVC(β= -0.34%,95%CI,-0.42% ~ -0.27%)和FVC(β= -0.18 L,95%CI,-0.32 L ~ -0.04 L)显著降低相关。
总之,在人群水平上,研究中考虑的职业暴露似乎不是肺功能差异的主要决定因素,尽管它们与更多的呼吸道症状相关。由于研究并未包括所有工作环境,仍应鼓励高危粉尘和烟雾作业工人进行呼吸监测,尤其是在低收入和中等收入国家。
原文出处:
Ratanachina J, Amaral AFS, De Matteis S, et al. Association of respiratory symptoms and lung function with occupation in the multinational Burden of Obstructive Lung Disease (BOLD) study. Eur Respir J 2022; https://doi.org/10.1183/13993003.00469-2022.

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#呼吸道症状#
50
#相关性#
40
好文章,谢谢分享。
42
#呼吸道#
53
#相关性分析#
46