肺动脉高压和肺静脉闭塞性疾病的双能CT肺灌注特征是什么?
2022-03-18 刘少飞 MedSci原创
比较肺动脉高压和肺静脉闭塞性疾病和/或肺毛细血管瘤病 的双能CT(DECT)灌注特征,特别关注PE型灌注缺损。
在对肺动脉高压(PAH)的潜在原因进行分层时,目前的指南建议进行 V/Q 肺闪烁扫描以筛查 CTEPH。CTEPH 的识别是基于对没有灌注但保持通气的肺段或亚段的识别。在一小部分特发性肺动脉高压 (PAH) 和肺静脉闭塞性疾病和/或肺毛细血管瘤病 (PVOD/PCH) 中也存在不匹配的灌注缺陷。尚未在这两个实体中专门研究双能 CT 肺灌注变化。
研究目的:比较 PAH 和 PVOD/PCH 的双能 CT (DECT) 灌注特征,特别关注 PE 型(即三角灌注缺损上的空气滞留)灌注缺损。
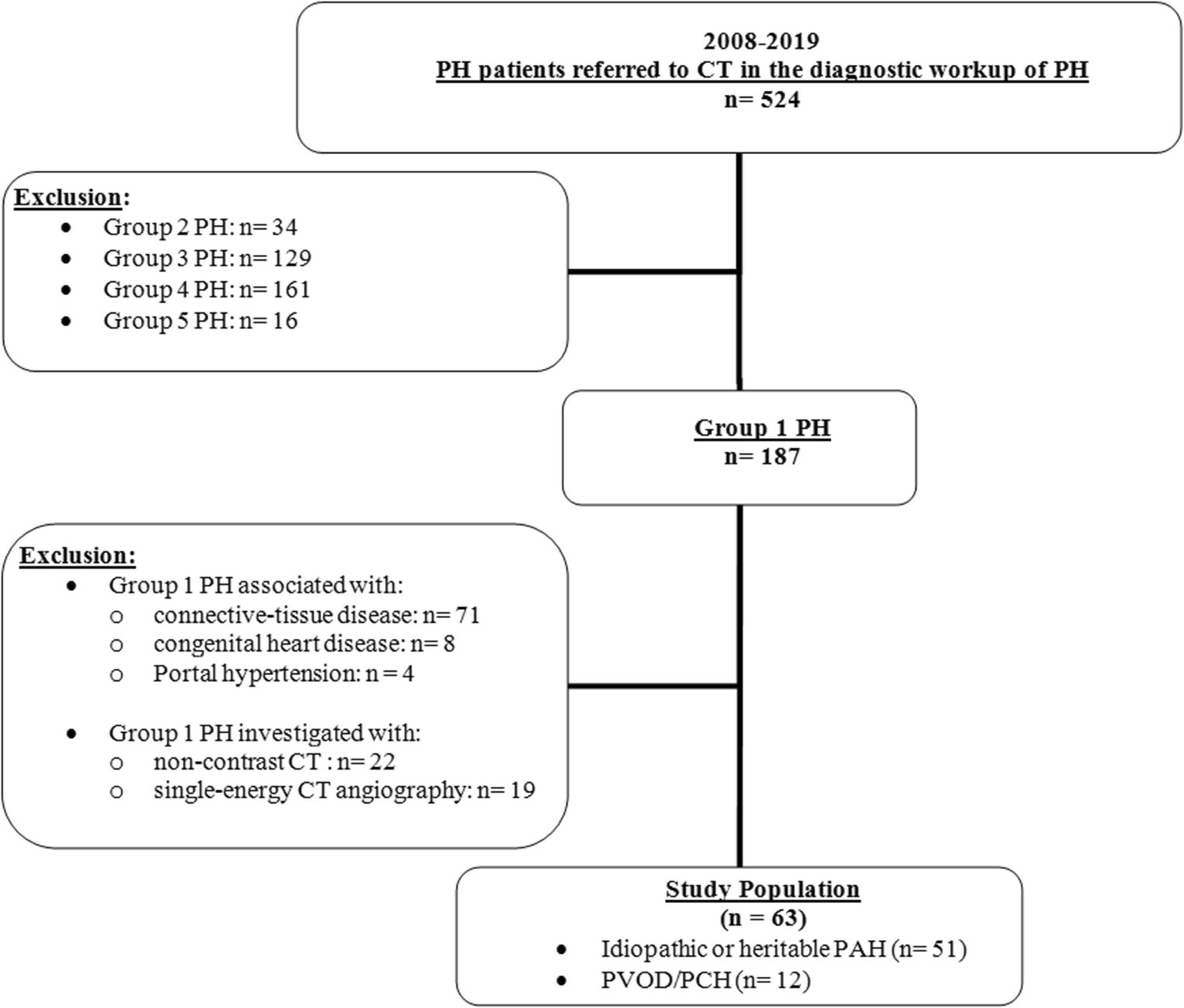
研究方法:对 63 名患有特发性或遗传性 PAH(A 组;n = 51)和 PVOD/PCH(B 组;n = 12)的患者进行了 DECT 血管造影以及形态学和灌注图像重建。
研究结果:
A组(35/51;68.6%)和B组(6/12;50%)( p = 0.31)之间灌注异常的患者数量没有差异,每名患者灌注异常的平均节段数也没有差异( A 组:17.9 ± 4.9;B 组:18.3 ± 4.1;p = 0.91)。最常见的发现是 A 组存在斑片状缺陷(15/35;42.9%)和 B 组灌注异常的可变关联(4/6;66.7%)。B 组每名患者出现 PE 型缺损的中位百分比显着高于 A 组(p= 0.041)。8 名患者(A 组:5/51;9.8%;B 组:3/12;25%)描述了两种类型的 PE 型缺陷,叠加在 PH 相关的肺异常(7/8)或正常肺( 1/8)。灌注异常患者的碘浓度显着降低(p < 0.001),但组间没有差异。
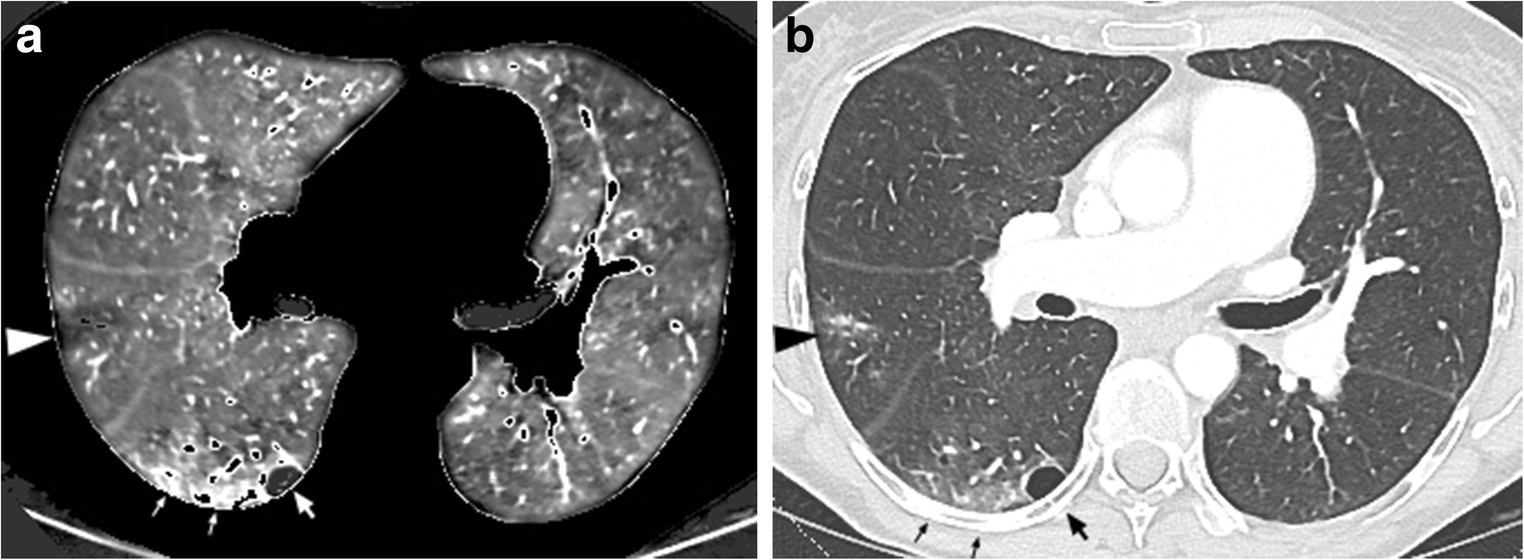
一名 52 岁、不吸烟的特发性 PAH 女性患者的双能 CT 检查。在右中间支气管水平获得的1 毫米厚的横向灌注图像,显示右上叶(箭头)有三角形楔形灌注缺损,双肺有许多斑片状缺损。注意右下叶心尖段的依赖肺灌注增加(细箭头),毗邻胸膜下大疱(粗箭头)。b,1 mm 厚的横向 CT 切片(肺图像),与a所示水平相同. 右上叶结节浸润叠加在 PE 型灌注缺损上(箭头)。与重力相关的右下叶依赖肺的磨玻璃样衰减(细箭头)。大箭头指向相邻的胸膜下大疱
研究结论:
除了 PVOD/PCH 患者中 PE 型缺损的节段中位数百分比较高外,两组之间的灌注异常没有差异。
参考文献:
Lefebvre B. Dual-energy CT lung perfusion characteristics in pulmonary arterial hypertension (PAH) and pulmonary veno-occlusive disease and/or pulmonary capillary hemangiomatosis (PVOD/PCH): preliminary experience in 63 patients. Eur Radiol. 2022 Mar 14. doi: 10.1007/s00330-022-08577-x. Epub ahead of print. PMID: 35286410.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#双能CT#
53
#动脉高压#
50
#静脉#
0
学习一下
53
#学习#学习
60
不错,学习了。
65