JAMA Pediatr:儿童急性阑尾炎使用抗生素治疗好还是阑尾切除术好?
2017-04-07 MedSci MedSci原创
使用抗生素治疗急性无并发症的阑尾炎对成年患者是有效的,但其在儿科患者中的应用仍有争议。近期,一项旨在比较抗生素治疗与阑尾切除术治疗儿童急性无并发症尾炎的安全性和疗效的研究发表在杂志JAMA Pediatr上。此项研究检索了2016年4月17日前PubMed、MEDLINE、EMBASE和Cochrane图书馆数据库以及Cochrane对照试验的随机临床试验。搜索仅限于以英文发表的研究。搜索词包括阑
使用抗生素治疗急性无并发症的阑尾炎对成年患者是有效的,但其在儿科患者中的应用仍有争议。
此项研究检索了2016年4月17日前PubMed、MEDLINE、EMBASE和Cochrane图书馆数据库以及Cochrane对照试验的随机临床试验。搜索仅限于以英文发表的研究。搜索词包括阑尾炎、抗生素、阑尾切除术、随机对照试验、对照临床试验、随机、安慰剂、药物治疗、随机和试验。
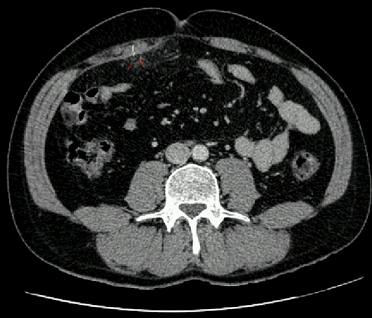
荟萃分析包括随机临床试验和比较抗生素治疗与阑尾切除术对儿科患者(5〜18岁)急性无并发症阑尾炎的临床对照试验。结果包括以下术语中的至少2项:抗生素治疗和阑尾切除术的成功率,并发症,再入院率,住院时间,总花费和残疾日数。数据由2位评审员独立提取。根据Cochrane指南和Newcastle-Ottawa标准,对包括的研究的质量进行了检查。主要研究结果是治疗的成功率。
此项荟萃分析显示,抗生素作为初步治疗小儿无并发症的阑尾炎患者可能是可行有效的,并且不增加合并症的风险。然而,由阑尾炎的存在引起的失败率高于阑尾切除术。建议手术适用于无并发症的阑尾炎患者。
原始出处:
Huang L, Yin Y, et al. Comparison of Antibiotic Therapy and Appendectomy for Acute Uncomplicated Appendicitis in Children: A Meta-analysis. JAMA Pediatr. 2017 Mar 27. doi: 10.1001/jamapediatrics.2017.0057.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#DIA#
45
#切除术#
47
#PE#
41
还是手术切除吧。
82
治疗帮助很大
86
晓得了,长知识了
64
学习了
71
#抗生素治疗#
34
#急性阑尾炎#
40
学习一下知识
64