Acta Neuropathologica: 多发性硬化皮质灰质坏死信号的神经元特异性激活
2021-03-29 MedSci原创 MedSci原创
多发性硬化(MS)的进展阶段在病理学上的特征是白质(WM)中慢性脱髓鞘病变的积聚,WM中可变的轴突损伤和丢失,正常出现的WM中的弥漫性变化和皮质灰质病理的增加。
多发性硬化(MS)的进展阶段在病理学上的特征是白质(WM)中慢性脱髓鞘病变的积聚,WM中可变的轴突损伤和丢失,正常出现的WM中的弥漫性变化和皮质灰质病理的增加。GM病理程度与临床进展率、身体残疾和认知障碍的相关性好于MRI上的WM病变负荷,GM中的神经退行性变现在被认为是这种累积的不可逆临床残疾的主要驱动因素之一。神经元丢失、轴突损伤、突触功能障碍和丢失,都是导致这种GM神经退行性病变的原因。然而,皮层神经退行性变和随后的GM萎缩的机制仍不清楚,尽管这可能是由慢性炎症引发的一系列事件所刺激的。
持续暴露于软脑膜中的促炎细胞因子被认为在导致MS皮质病理的发病机制中起主要作用。尽管灰质神经退行性变的分子机制尚不清楚,但一些证据表明肿瘤坏死因子(TNF)起着重要作用。

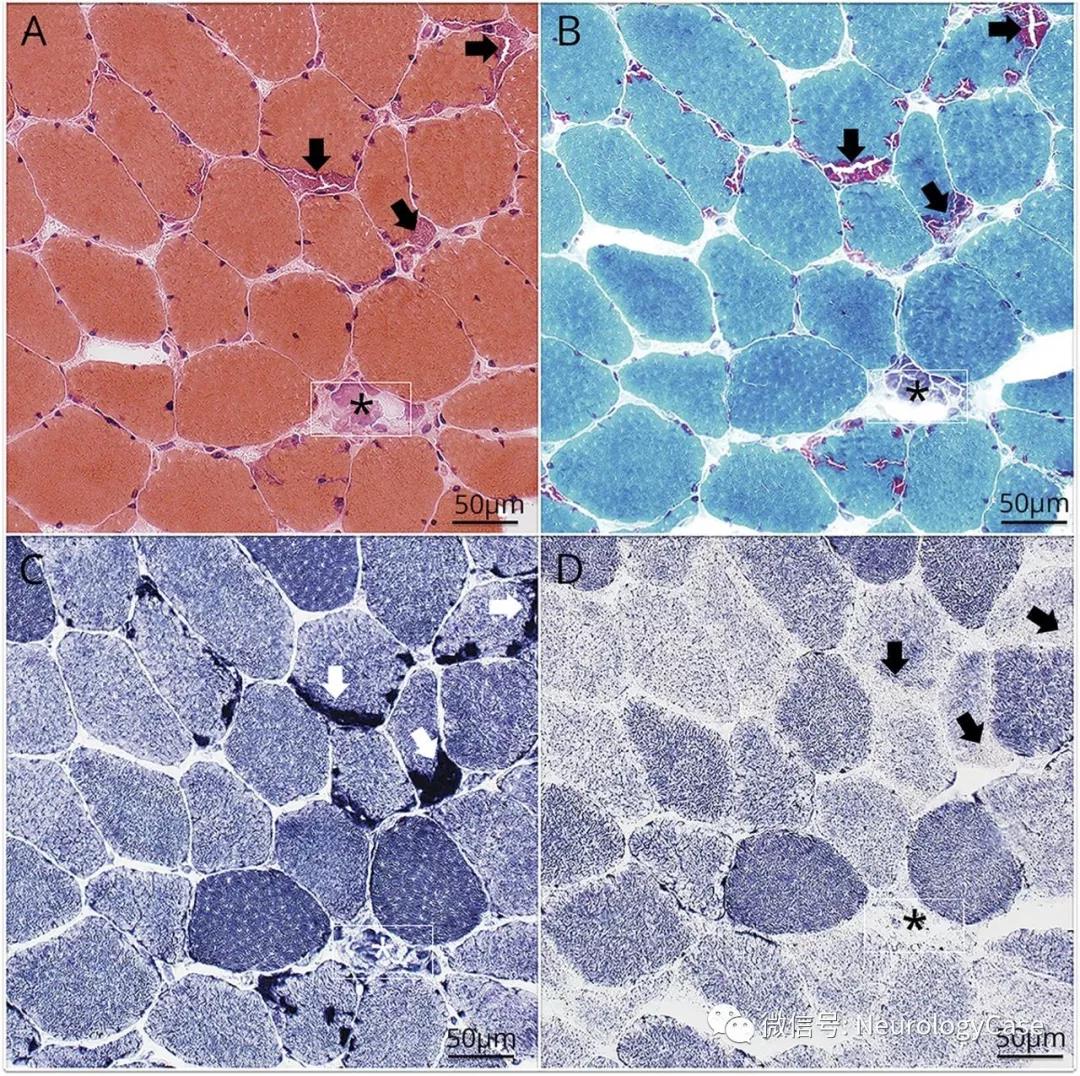
本文通过28例继发性进行性MS患者和10例非神经系统疾病对照者死后大脑皮质灰质组织块,描述了导致坏死的TNF/TNF受体1信号通路中多个步骤的表达增加,包括关键蛋白TNFR1、FADD、RIPK1、RIPK3和MLKL。RIPK3和MLKL的磷酸化以及坏死小体特有的蛋白质寡聚体的形成表明了该通路的激活。
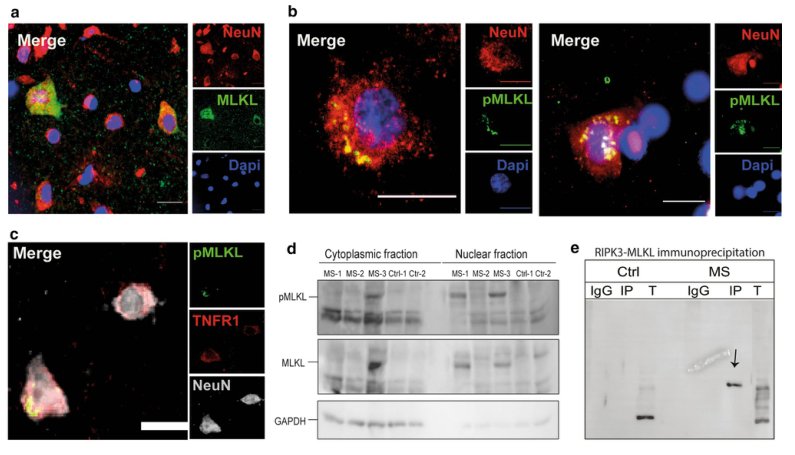
MS皮质灰质MLKL活化与坏死形成
相反,caspase-8依赖的凋亡信号转导减少。坏死信号的上调主要发生在皮质层II-III的宏观神经元中,在其他细胞类型中几乎没有表达。在伴有显著脑膜炎症的MS患者中,神经元中活化坏死蛋白的存在增加,第Ⅰ至第III层的磷酸化MLKL+神经元增加了30倍。
磷酸化MLKL+神经元的密度与死亡年龄、进展年龄和疾病持续时间呈负相关。在大鼠模型中,通过脑膜中的慢病毒转导,体内诱导脑脊液中的肿瘤坏死因子和干扰素γ水平长期升高,触发了底层皮质灰质的炎症和神经退行性变,这与TNFR1和活化的坏死信号蛋白的神经元表达增加有关。
本文的研究数据表明,MS皮质中的神经元通过TNF/TNFR1刺激的坏死而不是凋亡而死亡,这可能部分是由慢性脑膜炎症引起的。神经元坏死代表了一种发病机制,可在信号通路的几个点进行治疗干预。
Picon, C., Jayaraman, A., James, R. et al. Neuron-specific activation of necroptosis signaling in multiple sclerosis cortical grey matter. Acta Neuropathol 141, 585–604 (2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Pathol#
32
#CTA#
0
#多发性#
25
#特异性#
31
#pathologic#
32
#坏死#
26