肺动脉高压中血流动力学和壁力学及其相互作用
2021-11-23 刘少飞 MedSci原创
血管壁硬度和血液动力学参数是检测肺动脉高压(PAH)的潜在生物力学标志物。然而,以前的计算分析没有考虑血流和壁变形之间的相互作用。在这里,应用既定计算框架,分析PAH及对照近端血流与血管壁相互作用。
肺动脉高压 (PAH) 是一种复杂的心血管疾病,其特征是肺动脉进行性重塑。这一持续过程由肺动脉 (PA) 压力增加促进,导致右心房功能障碍、右心室 (RV) 肥大和心室-血管耦合受损。虽然 PAH 的末期是右心衰竭,但这主要是由肺血管系统的发病机制驱动的。由于环境高度复杂,心肺系统适应不利条件的能力强,起病症状通常较轻,可能难以识别。因此,PAH 患者通常在晚期被诊断出来,恶化速度更快(从确诊到治疗失败一般3-5 年)和更高的死亡率(5 年内死亡率29%)。临床指导建议早期发现可以大大增加生存机会。因此,迫切需要进一步了解导致疾病进展的机制,以帮助识别 PAH 检测的新生物力学标志物,尤其是在早期阶段。最近的证据表明,PA 中的血管硬化、右心房 (RA) 和 RV 功能以及血流动力学可以作为检测 PAH 和预测其进展的潜在生物力学标志物。 在血管硬化方面,已经提出了诸如脉搏波速度、函数、相对面积变化(RAC)、刚度指数和PA扩张性等参数。 然而,这些指数无法区分与血管硬化相关的几何和材料变化的影响,即,它们无法评估血管壁固有机械特性的变化,这被认为是血管硬化的主要驱动因素之一。
已经提出了其他非侵入性 PA 血流动力学测量,例如,体积流量波形轮廓的变化。具体而言,在 PAH 的 PA 中发现的逆流模式已被建议作为潜在的生物标志物,因为它可以在其他 PAH 指标之前被识别。此外,近端 PA 的低壁剪切应力 (WSS) 被认为是 PAH 严重程度的良好指标,因为它已被证明在 PAH 的发病机制中发挥作用。然而,其中一些建议是基于计算分析提出的,假设顺应PA壁是刚性的,这是之前讨论过的一个限制。其他描述患者特异性血管壁-血流动力学相互作用的计算模型最近已用于研究单个成人或儿童患者队列的 PAH。然而,只有少数研究调查了一组成年患者的血流动力学-壁力学关系。因此,本研究的目的是通过利用我们先前开发的患者特异性流体结构相互作用 (FSI) 框架,在 6 名 PAH 患者和 5 名对照受试者的近端 PA 动脉处引发血管壁力学和血流动力学相互作用。该框架最初用于评估 PAH 患者和对照受试者的局部血液动力学-壁力学相互作用,用于量化多个成年 PAH 患者的线性弹性模量、壁表面位移、血液动力学以及远端血管顺应性和阻力.
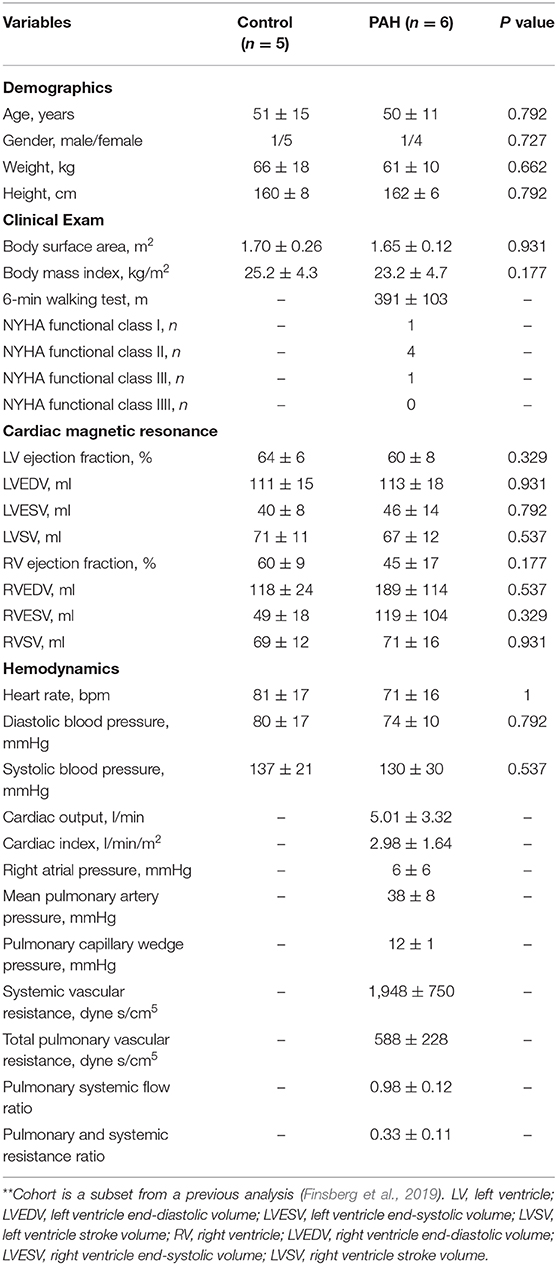
研究患者队列:
使用带有 ECG 门控的 3-Tesla Philips 扫描仪从基于导管插入术诊断为 PAH 的 6 名患者采集电影和相差 (PC) 磁共振 (MR) 图像。使用 Q-Flow 软件(飞利浦医疗系统)从 PC-MR 图像对主肺动脉 (MPA) 的血流速度和体积流量进行后处理。还使用标准技术对 PAH 患者在休息时(影像学检查后 1 周内)进行了右心导管插入术 (RHC)。五名没有已知心血管疾病或其他合并症的人类受试者在本研究中作为对照,并且还接受了从中获取电影 MR 图像的 MR 成像。
研究结果:
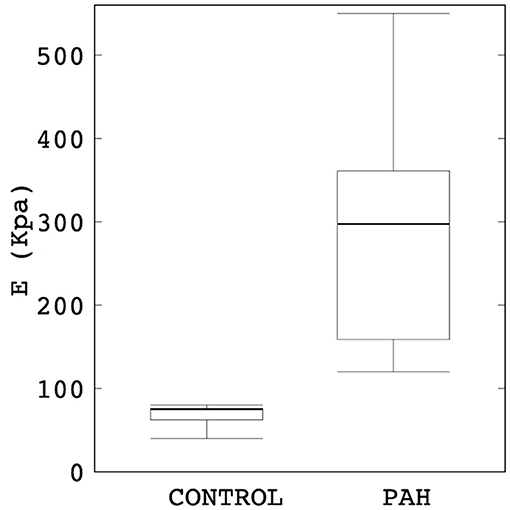
动脉壁力学
发现 PAH 组中主肺动脉(MPA)的舒张末期直径显着大于对照组(28%)。 另一方面,与对照组相比,PAH 组的 RAC 也显着降低(约 50%)。

与对照组相比,发现 PAH 组的线性 PA 刚度 E 显着更高(约四倍)。 对照组中 E 的四分位距也明显小于 PAH 组。
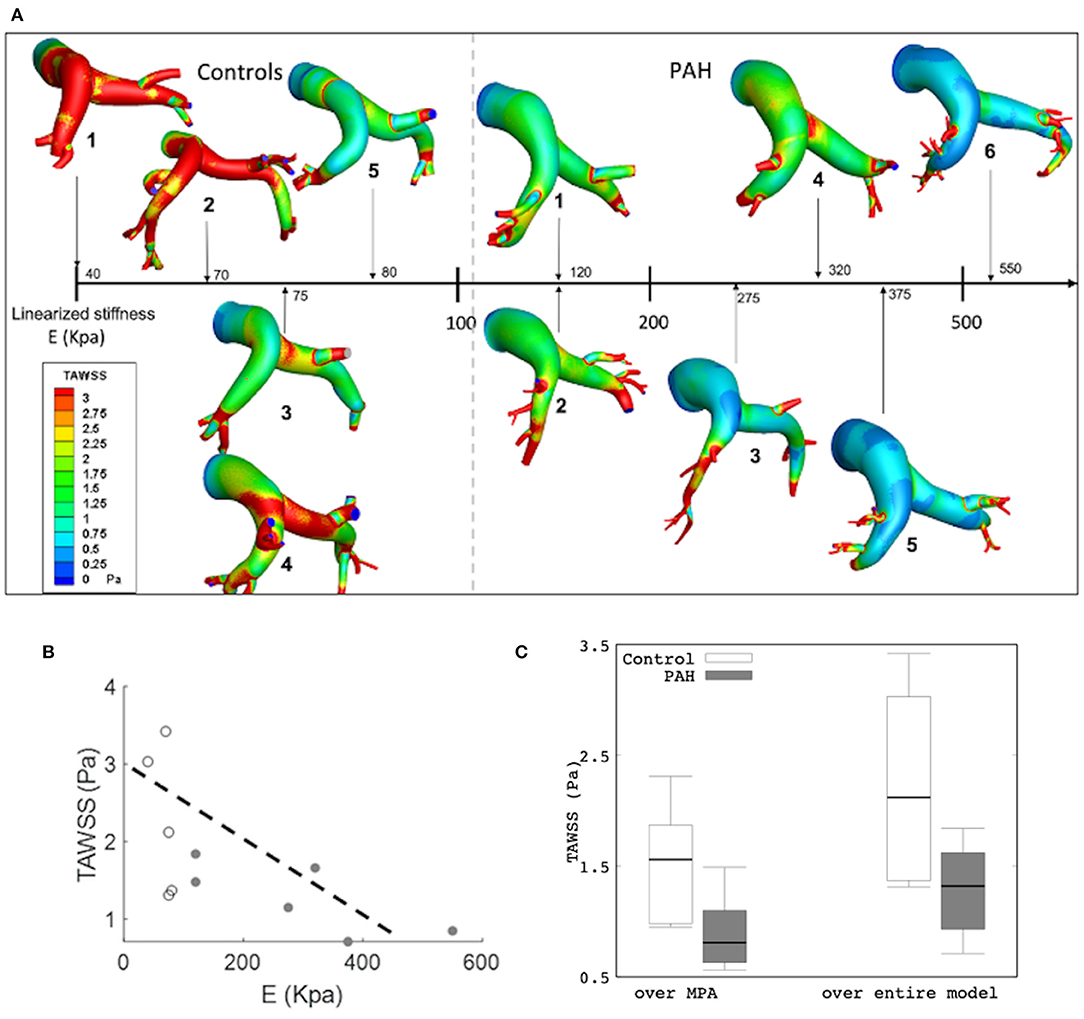
血流动力学
体积流量波形分析(使用 PC-MRI 在近端 PA 测量)显示所有 PAH 患者在收缩期后都有反流(回流)。 发现反流流量随着线性刚度 E 的增加而增加。 在一个心动周期内 MPA 中的反流流量总量与模型估计的线性弹性模量 E 之间发现了很强的线性相关性。

模拟结果还显示所有患者中 TAWSS 的空间分布存在差异。 平均而言,对照组的平均 TAWSS 高于 PAH 组。 与最大表面位移和线性弹性模量 E 之间的关系类似,TAWSS 随着 E 的增加而降低。具体而言,PAH 中整个 PA 和 MPA 段的平均 TAWSS 低于对照组。 当考虑所有受试者(PAH + 对照)时,整个 PA 和 MPA 的平均 TAWSS 显示出与线性刚度 E 的强相关性。 然而,当仅考虑 PAH 患者时,整个 PA 的平均 TAWSS 与大肠杆菌密切相关。
研究启示:
该研究应用特定于患者的计算框架来研究 6 名 PAH 患者和 5 名对照受试者的 PA 中血管壁力学和血流动力学之间的相互作用。 主要发现如下:(1) PAH 患者的线性弹性模量 E 与对照组相比显着升高,(2) E 与 PA 中的总反流流量直接相关,(3) TAWSS 与 PAH 患者线性弹性模量 E 的增加呈负相关,并且 (4) 远端阻力 Rt 和顺应性 Ct 分别随 PAH 升高和降低。
文献出处:
Zambrano BA, McLean N, Zhao X, Tan JL, Zhong L, Figueroa CA, Lee LC, Baek S. Patient-Specific Computational Analysis of Hemodynamics and Wall Mechanics and Their Interactions in Pulmonary Arterial Hypertension. Front Bioeng Biotechnol. 2021 Jan 28;8:611149. doi: 10.3389/fbioe.2020.611149. PMID: 33634080; PMCID: PMC7901991.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#相互作用#
48
#动脉高压#
39
#血流动力#
48
#血流动力学#
37
#互作#
42
谢谢
58