JAHA:柠檬酸镁、氧化镁和硫酸镁补充剂对动脉僵硬度的影响
2022-03-07 MedSci原创 MedSci原创
口服柠檬酸镁治疗24周并没有显著改变动脉僵硬度或血压。氧化镁和硫酸镁具有相似的非显著效应。
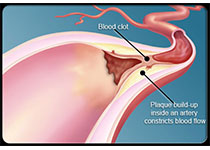
动脉僵硬度是冠心病和卒中的独立预测因素。虽然动脉硬化随着年龄的增长而增加,但生活方式的改变,如减肥和减少饮食盐和酒精的摄入量已被证明可以减少动脉硬化。此外,增加膳食镁摄入量可能会改善动脉僵硬度。镁补充剂可能对动脉僵硬度有益。然而,目前尚未有研究对各种镁制剂对动脉僵硬度的影响进行直接比较。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员评估了柠檬酸镁补充剂对动脉僵硬度和血压的影响,并探讨了其他镁制剂是否具有类似的效果。

在这项随机试验中,超重和轻微肥胖的受试者接受柠檬酸镁、氧化镁、硫酸镁或安慰剂治疗24周。镁的每日总剂量为450mg/天。该研究的主要结局是颈动脉到股动脉的脉搏波速度,这是测量动脉硬度的金标准。该研究的次要结局包括血压、血浆和尿镁。

总体而言,该研究纳入了164名参与者(平均±SD年龄为63.2±6.8岁;104名[63.4%]女性)。在意向治疗分析中,与安慰剂相比,柠檬酸镁和其他制剂在24周时对颈股动脉脉搏波速度或血压均无影响。与安慰剂相比,柠檬酸镁可增加血镁(+0.04mmol/L;95%CI,+0.02至+0.06mmol/L)和尿镁(+3.12mmol/24h;95%CI,+2.23至+4.01mmol/24h)浓度。镁补充剂组对血浆镁的影响相似,但与氧化镁或硫酸镁相比,柠檬酸镁导致24小时尿镁排泄量增加更显著。该研究共报告了一起严重的不良事件,这被认为与研究治疗无关。
由此可见,口服柠檬酸镁治疗24周并没有显著改变动脉僵硬度或血压。氧化镁和硫酸镁具有相似的非显著效应。
原始出处:
Joëlle C. Schutten.et al.Effects of Magnesium Citrate, Magnesium Oxide, and Magnesium Sulfate Supplementation on Arterial Stiffness: A Randomized, Double‐Blind, Placebo‐Controlled Intervention Trial.JAHA.2022.https://www.ahajournals.org/doi/full/10.1161/JAHA.121.021783
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#AHA#
37
#硫酸镁#
51
#柠檬酸#
44
#动脉僵硬#
44
#动脉僵硬度#
52