新型 p38 丝裂原活化蛋白激酶抑制剂可逆转缺氧诱导的大鼠肺动脉高压
2022-07-30 刘少飞 MedSci原创
本工作研究了LASSBio-1824在缺氧+SU5416诱导的(SuHx)PH大鼠心肺系统结构和功能的病理生理变化中的药理作用。
肺动脉高压 (PH) 是一种临床病症,其中观察到肺血管重塑和阻塞,最终导致肺动脉阻力和压力显着升高。它影响着全世界大约 10% 的老年人口,每年每百万人中有 3-10 例新病例被诊断出来,主要是年轻女性。如果不使用适当的治疗,预计平均生存期为 2.8 年,即使考虑到治疗的最新进展,诊断 5 年后生存率仍仅为 61%。
丝裂原活化蛋白激酶 (MAPK) 通过调节细胞增殖、分化、存活和组织炎症触发多种疾病的病理生理机制。p38 的抑制在 PH 和 RV 衰竭的动物模型中显示出有益效果。p38 的激活与炎症介质的产生有关,例如肿瘤坏死因子 (TNF)-α 和诱导型一氧化氮合酶 (iNOS)。此外,p38 还调节半胱天冬酶介导的细胞凋亡,这是 PH 期间参与血管重塑的重要条件。此外,该 MAPK还证明了在 RV 肥大和压力过载反应功能障碍中的独立作用。因此,心肺系统中的 p38 抑制可以直接在 RV 和肺中促进有益作用,并具有轻微的全身副作用。
最近,报道了 ( E ) -N '-(4-(pyridin-2-yl)benzylidene)-2-naphthohydrazide (LASSBio-1824,图 1 ) 的合成。这种新的N-酰基腙衍生物在体外生化试验中抑制 p38,并在小鼠口服给药后在体内显示出抗炎活性。基于此,本工作研究了LASSBio-1824在缺氧+SU5416诱导的(SuHx)PH大鼠心肺系统结构和功能的病理生理变化中的药理作用。

图 1. LASSBio-1824 的分子结构
丝裂原活化蛋白激酶 (MAPK) 信号传导与肺动脉高压 (PH) 和右心室 (RV) 衰竭的心血管重塑密切相关。在实验诱导的 PH 中研究了新设计的 p38 抑制剂 LASSBio-1824 的作用。雄性 Wistar 大鼠暴露于缺氧和 SU5416 (SuHx) 环境中,并使用常氧大鼠作为对照。
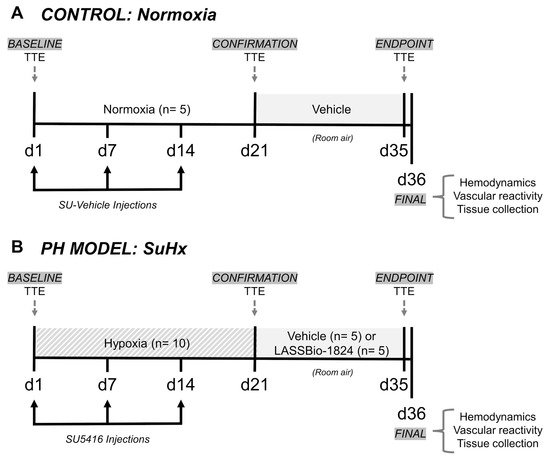
图 2. 模型诱导、治疗方案和测量计划
使用载体或 LASSBio-1824 (50 mg/kg) 进行 14 天的口服治疗。通过超声心动图和导管插入术评估肺血管阻力和右室结构和功能。对肺和 RV 进行组织学、免疫组织化学和蛋白质印迹分析,以研究心血管重塑和炎症。LASSBio-1824 治疗通过减轻血管肌化和内皮功能障碍使血管阻力正常化。在心脏,治疗降低了 RV 收缩压、肥大和胶原蛋白含量,改善了心脏功能。治疗后肺血管和右室组织中 TNF-α、iNOS、磷酸化 p38 和 caspase-3 的蛋白质含量降低,并且在治疗的 SuHx 大鼠的心肌细胞中发现转录因子 c-fos 的激活降低。因此,LASSBio-1824 代表了重塑靶向治疗 PH 的潜在候选药物。
研究结论:
这项工作的新颖之处在于证明了一种新型口服活性 p38 抑制剂对慢性缺氧加 SU5416 诱导的 PH 大鼠的有益作用。在 14 天内用 LASSBio-1824 口服治疗可降低 PH 特征,包括肺动脉中血流和内皮功能的改变以及肺血管和 RV 中的组织重塑。LASSBio-1824 对 p38 的抑制作用通过降低 TNF-α 和 iNOS 的表达来减轻组织炎症,并通过抑制 c-fos 和 caspase-3 的激活来防止 RV 组织对应激的细胞凋亡。LASSBio-1824 促进的作用有助于肺和 RV 修复,这加强了将 p38 MAPK 作为治疗 PH 的有希望的靶点的重要性
参考文献:
Silva GF, da Silva JS, de Alencar AKN, de Moraes Carvalho da Silva M, Montagnoli TL, de Souza Rocha B, de Freitas RHCN, Sudo RT, Fraga CAM, Zapata-Sudo G. Novel p38 Mitogen-Activated Protein Kinase Inhibitor Reverses Hypoxia-Induced Pulmonary Arterial Hypertension in Rats. Pharmaceuticals (Basel). 2022 Jul 21;15(7):900. doi: 10.3390/ph15070900. PMID: 35890198.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#蛋白激酶#
41
#抑制剂#
77
#激酶抑制剂#
43
#动脉高压#
34
#激酶#
52