Hepatology:HBsAg血清学清除的发生率和预测因素!
2017-11-15 MedSci MedSci原创
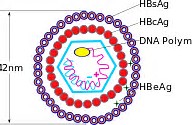
在核苷(酸)类似物(Nuc)治疗期间,乙型肝炎表面抗原(HBsAg)丧失较为罕见。目前,仅有有限的数据表明,停止Nuc治疗可能会增加乙型肝炎e抗原(HBeAg)阴性患者的HBsAg的消失率。近期,一项发表在杂志Hepatology上的研究详细地调查这个问题。在Nuc治疗156(61-430)周的1075例HBeAg阴性患者中,6例在治疗过程中出现HBsAg血清学清除,估计年发生率为0.15%。在H
在核苷(酸)类似物(Nuc)治疗期间,乙型肝炎表面抗原(HBsAg)丧失较为罕见。目前,仅有有限的数据表明,停止Nuc治疗可能会增加乙型肝炎e抗原(HBeAg)阴性患者的HBsAg的消失率。
近期,一项发表在杂志Hepatology上的研究详细地调查这个问题。
在Nuc治疗156(61-430)周的1075例HBeAg阴性患者中,6例在治疗过程中出现HBsAg血清学清除,估计年发生率为0.15%。在HBsAg血清阳性的患者中,691例(52.3岁,86%男性,44.6%肝硬化)停止了Nuc治疗,随后进行了前瞻性随访。
在155(2-614)周的中位治疗后随访期间,42例患者确诊为HBsAg血清学清除。6年累计发病率为13%,预计年发病率为1.78%。Cox回归分析显示,HBV DNA检测不到的时间较短(<12wks),治疗期间HBsAg降低较多(> 1 log10),EOT HBsAg水平较低(<100 IU/mL),持续应答和复发而未恢复的患者是不再进行治疗的HBsAg血清学清除的因素。
此项研究结果表明:停用Nuc后,HBsAg血清学清除的发生率远远高于治疗期间,且无病毒学和临床复发的患者中HBsAg血清清除率最高。未经治疗的临床复发患者HBsAg清除发生率比接受再治疗的患者高7.34倍,这也提示短暂的未经治疗的临床复发可能导致足够的免疫控制从而达到功能的治愈。
原始出处:
Jeng WJ, Chen YC, et al. Incidence and predictors of HBsAg seroclearance after cessation of nucleos(t)ide analogue therapy in HBeAg negative chronic hepatitis B. Hepatology. 2017 Nov 6. doi: 10.1002/hep.29640.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#发生率#
32
#预测因素#
31
#HBsAg#
31
#EPA#
29
#血清学#
0