Alzheimer Dementia:认知损害的人,黄斑变性的可能性更大
2021-12-08 Freeman MedSci原创
认知障碍与AREDS2中的晚期AMD进展有关,这强调了认知障碍者的眼睛护理的重要性。
年龄相关性黄斑变性(AMD)是一种涉及中央视网膜(黄斑)损伤的眼病,是美国法定失明的最常见原因。2020年,全世界有1.96亿人受到AMD的影响;其中1100万人患有晚期AMD(即晚期AMD,一个疾病阶段,人们也开始出现有症状的视力下降)。
预计到2040年,负担将分别增加到2.88亿人和1900万人。AMD是由环境因素和遗传学之间复杂的相互作用产生的,晚期AMD造成的不可逆的视力丧失会导致生活质量下降和丧失独立性。认知障碍是导致老年人残疾的另一个与年龄有关的原因,通常是渐进的和不可逆的。随着老年人数量的增加,更好地了解导致认知功能损害和痴呆综合症(包括阿尔茨海默病[AD])的风险因素至关重要。
不同强度的证据显示,AD和AMD作为老龄化的神经退行性疾病之间存在关联,但这仍有争议。两者可能在某种程度上共享关键的环境风险因素(如饮食)、组织病理学特征(如淀粉样β[Aβ]的沉积)和病理生理机制(如氧化压力和炎症)。然而,他们的遗传风险状况是不同的;唯一已知的共同基因座是脂蛋白E(APOE)ε4,它与AD的风险增加有关,但可能对发展到晚期AMD有保护作用。
美国国家眼科研究所赞助的老年性眼病研究(AREDS)和AREDS2是多中心、随机临床试验(RCTs),用于治疗AMD和白内障的营养补充剂。AREDS和AREDS2揭示了每日高剂量抗氧化维生素、矿物质和营养素组合的好处,可适度降低从中度到晚期AMD的进展风险。
在AREDS中,调查人员先前记录了AMD和老年人认知障碍之间的潜在联系。这项分析是横断面的,然而AMD和认知障碍之间的关联方向还不清楚。在AREDS2中,调查人员在基线和整个研究访问期间定期测试认知能力,使用的认知功能量表不依赖于需要视觉输入的测试。该试验显示,AREDS2补充剂对认知结果没有影响。
藉此,美国国立卫生研究院的Jimmy T. Le等人,探究了参加AREDS2的中晚期AMD老年人的认知障碍和晚期AMD之间的双向关系。值得注意的是,AREDS2(通过对认知功能的辅助研究和10年的随访21)是最大的老年人研究之一,具有长期随访(中位数为10年)和低随访损失(2%)。
老年性眼病研究2(AREDS2)的参与者每年都要接受眼科检查和认知功能测试(例如,改良的认知状态电话访谈[TICS-M])。他们还研究了认知障碍(如TICS-M得分<30)与5年和10年后的晚期AMD之间的双向关系。
他们分析了5189只眼睛(3157名参与者;平均年龄72.7岁),并对其进行了10.4年的中位跟踪。
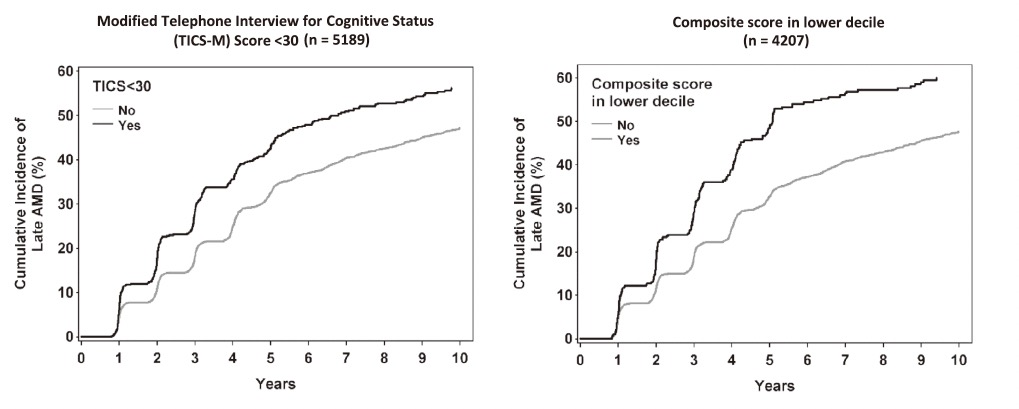
与没有认知障碍的参与者相比,基线上有认知障碍的参与者的眼睛在5年(危险比[HR],1.24;95%置信区间[CI],1.08-1.43)和10年(HR,1.20;95%CI,1.05-1.37)更有可能发展成晚期AMD。
基线AMD严重程度较差与发展认知障碍没有关系。
这个研究的重要意义在于发现了:认知障碍与AREDS2中的晚期AMD进展有关,这强调了认知障碍者的眼睛护理的重要性。
原文出处:
Le JT, Agrón E, Keenan TDL, et al. Assessing bidirectional associations between cognitive impairment and late age‐related macular degeneration in the Age‐Related Eye Disease Study 2. Alzheimer’s & Dementia. Published online November 10, 2021:alz.12473. doi:10.1002/alz.12473
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#dementia#
32
感谢分享
59
已学习
53
学习了
45
受益匪浅
60
学习了
48
学习了
35
学习了
33
学习了
30
#变性#
32