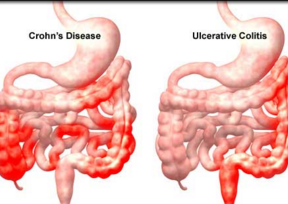
Am J Gastroenterol:brodalumab会导致活动性克罗恩病恶化
2016-08-09 Seven L 译 MedSci原创
目的:评估人抗白介素17受体单克隆抗体brodalumab治疗中度至重度克罗恩氏病(CD)的有效性和安全性。方法:第二阶段随机双盲安慰剂对照试验将患者按1∶1∶1∶1随机分为brodalumab(210、350或700 mg)或安慰剂组。第六周达到克罗恩病活动指数(CDAI)缓解(≤150)的比例作为主要结局指标。继发结局指标包括CDAI反应比例和变化情况。结果:因治疗组CD恶化,研究提前终止。终
目的:评估人抗白介素17受体单克隆抗体brodalumab治疗中度至重度克罗恩氏病(CD)的有效性和安全性。
方法:第二阶段随机双盲安慰剂对照试验将患者按1∶1∶1∶1随机分为brodalumab(210、350或700 mg)或安慰剂组。第六周达到克罗恩病活动指数(CDAI)缓解(≤150)的比例作为主要结局指标。继发结局指标包括CDAI反应比例和变化情况。
结果:因治疗组CD恶化,研究提前终止。终止时130名患者进行了分析。第六周,缓解率分比为3% (210 mg)、15% (350 mg)、9% (700 mg)和3% (安慰剂);CDAI反应率分别为16% (210 mg)、27% (350 mg)、15% (700 mg)和13% (安慰剂);平均CDAI变化为-8.7 (95.3) (210 mg)、-35.4 (105.6) (350 mg)、-0.6 (105.9) (700 mg)和-28.2 (86.0) (安慰剂)。除了治疗组患者CD病情恶化,其他不良事件的发生率在治疗组是类似的。
结论:使用brodalumab治疗导致不成比例的患者CD恶化,没有证据表明其有效性。除了活动性CD患者病情恶化外,没有发现brodalumab其他的安全性风险。
原始出处:
Targan SR.et al.A Randomized, Double-Blind, Placebo-Controlled Phase 2 Study of Brodalumab in Patients With Moderate-to-Severe Crohn's Disease.Am J Gastroenterol. 2016 Aug 2. doi: 10.1038/ajg.2016.298. [Epub ahead of print]
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#GAS#
27
#活动性#
30
#活动性克罗恩病#
39
#AST#
25
#Gastroenterol#
32
深度好文,值得学习
44
很好,不错,以后会多学习
39
#mAb#
26
深度好文,赞一个!!!
46
继续关注
44