实验性BTK抑制剂SAR442168可显著降低多发性硬化症的疾病活动
2020-04-23 Allan MedSci原创
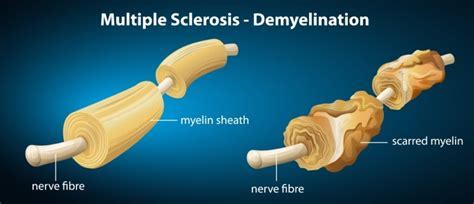
多发性硬化症(MS)是一种脱髓鞘性神经病变,患者脑或脊髓中的神经细胞表面的绝缘物质(即髓鞘)受到破坏,神经系统的信号转导受损,影响患者的活动、心智、甚至精神状态。
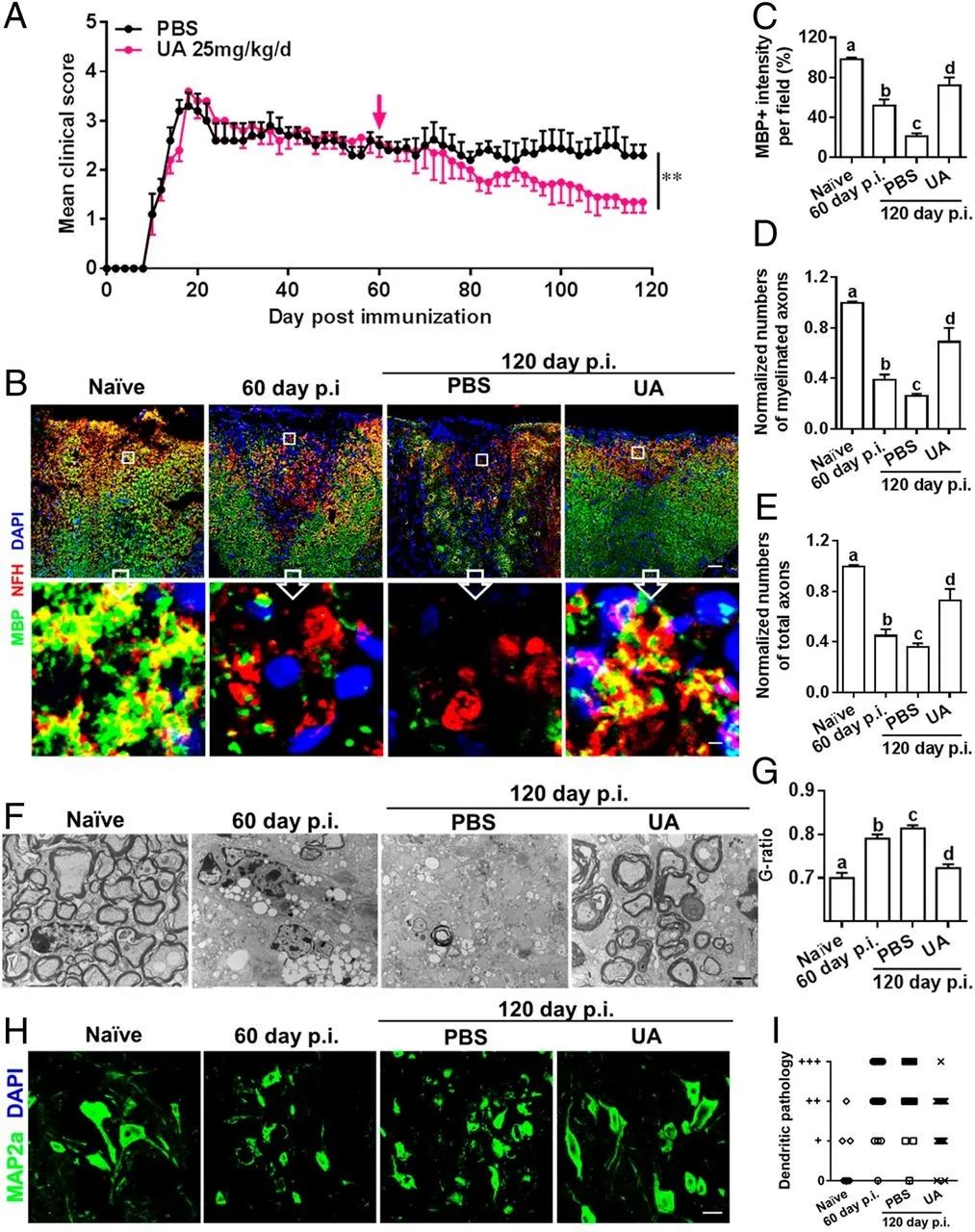
多发性硬化症(MS)是一种脱髓鞘性神经病变,患者脑或脊髓中的神经细胞表面的绝缘物质(即髓鞘)受到破坏,神经系统的信号转导受损,影响患者的活动、心智、甚至精神状态。赛诺菲今日宣布,在一项IIb期临床试验中,实验性BTK抑制剂SAR442168治疗复发性多发性硬化症(MS)使高强度病灶减少了85%。该公司在2月报道称,小分子选择性BTK抑制剂SAR442168达到了该试验的主要终点,显著降低了MS相关疾病活动。
赛诺菲全球研发部负责人John Reed说:“我们相信脑渗透性BTK抑制剂有望减少神经炎症和神经变性。在前进的过程中,我们将探索脑渗透性BTK抑制剂是否对复发性MS患者具有强大的疗效和出色的安全性。我们正在启动四个关键III期临床试验”。
这项IIb期研究的目的是通过MRI测量脑部病变的数量,评估5毫克至60毫克剂量的SAR442168治疗12周后的剂量-反应关系。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#抑制剂#
25
#多发性#
0
#硬化症#
0
#疾病活动#
29
#SAR442168#
37
#实验性#
30
#BTK抑制剂#
47
#BTK#
34