Radiology:女性和男性的胸主动脉直径和心血管事件的发生率及死亡率之间的关系
2022-09-02 shaosai MedSci原创
尽管胸主动脉扩张是临床实践中经常发现的问题,但在人群中很少有关于其对主要心血管疾病长期预后的作用的纵向数据。
 临床上发现,胸部主动脉扩张通常是无症状的,然而包括夹层或破裂等并发症的风险随着主动脉直径的增加而上升。因此,国际指南推荐的手术适应症主要是基于主动脉直径,并从权衡潜在的自然并发症的风险和选择性手术的风险中得出。然而,主动脉直径也随着年龄的增长而增加。血管大小和结构的变化(即血管重塑)具有系统性,涉及血液动力学和生物过程(氧化、炎症、基质降解、纤维化),在心血管疾病的发病机制中起关键作用。尽管胸主动脉扩张是临床实践中经常发现的问题,但在人群中很少有关于其对主要心血管疾病长期预后的作用的纵向数据。
临床上发现,胸部主动脉扩张通常是无症状的,然而包括夹层或破裂等并发症的风险随着主动脉直径的增加而上升。因此,国际指南推荐的手术适应症主要是基于主动脉直径,并从权衡潜在的自然并发症的风险和选择性手术的风险中得出。然而,主动脉直径也随着年龄的增长而增加。血管大小和结构的变化(即血管重塑)具有系统性,涉及血液动力学和生物过程(氧化、炎症、基质降解、纤维化),在心血管疾病的发病机制中起关键作用。尽管胸主动脉扩张是临床实践中经常发现的问题,但在人群中很少有关于其对主要心血管疾病长期预后的作用的纵向数据。
有限的现有纵向数据主要集中在主动脉根部,并表明主动脉根部直径与心血管疾病和死亡率有关联。只有两项研究调查了升胸主动脉(AA)或降胸主动脉(DA)与心血管事件之间的关系。此外,关于胸主动脉不同节段的扩张对不同心血管事件的长期预后价值的数据也很缺乏。因为主动脉直径与身体测量有很大关系,使用以身体测量为指数的主动脉直径可以提高其对心血管结局的预后价值。在无症状的女性和男性中评估与胸主动脉大小相关的心血管风险,可形成有效的性别特定预防策略。
近日,发表Radiology杂志的一项研究探讨了在胸部CT中心脏门控的AA和DA直径与随访期间女性和男性的心血管事件和死亡率之间的关系,为主动脉扩张的早期干预、减少并发症的发生提供了支持。
本研究对2003年至2006年期间接受多排CT检查的鹿特丹研究参与者进行了评估。进行了Cox比例危险模型来评估AA和DA直径与男性和女性的心血管事件和死亡率之间的关系,该模型是以体重指数(BMI)为索引和未以体重指数为索引。主动脉直径每大1个单位的SD计算危险比(HRs)。
共有2178名参与者(平均年龄69岁;55%为女性)被纳入研究。平均随访时间为9年。BMI指数的AA直径每大0.23mm/(kg/m2),女性的心血管死亡风险就会增加33%(HR,1.33;95% CI:1.03,1.73)。BMI指数DA直径每大0.16mm/(kg/m2)与女性卒中风险高38%(HR,1.38;95%CI:1.07,1.78)和心血管死亡风险高46%(HR,1.46;95%CI:1.10,1.94)有关。在男性和女性中,较大BMI指数的AA和DA直径与较大的全因死亡风险有关。
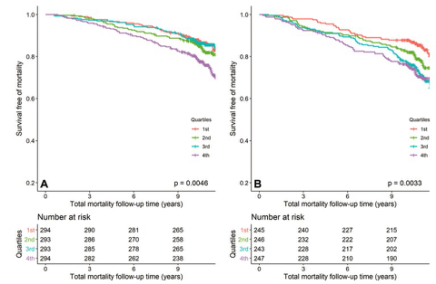
图 在女性和男性中,不同体重指数(BMI)指数的升主动脉(AA)直径四分位数的不良事件的Kaplan-Meier生存曲线。(A) BMI指数的AA直径和女性的总死亡率。(B) BMI指数的AA直径和男性的总死亡率
本研究结果表明,以体重指数为指标测量升主动脉和降主动脉的直径可以确定女性和男性的不良心血管结果和死亡的风险。
原文出处:
Oscar L Rueda-Ochoa,Lidia R Bons,Fang Zhu,et al.Thoracic Aortic Diameter and Cardiovascular Events and Mortality among Women and Men.DOI:10.1148/radiol.210861
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#胸主动脉#
0
#血管事件#
43
#发生率#
42
#主动脉#
43