Sci Transl med:白血病患者福音!新发现有望提高“造血干细胞移植”成功率
2018-11-30 探索菌 生物探索
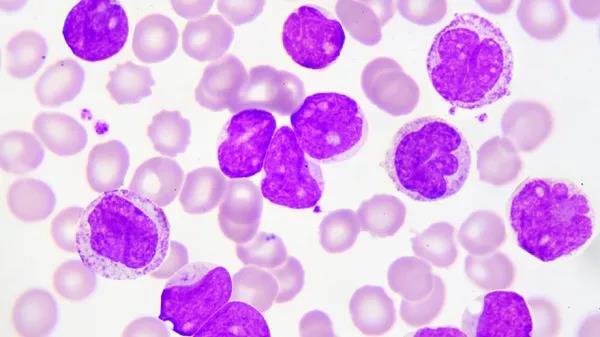
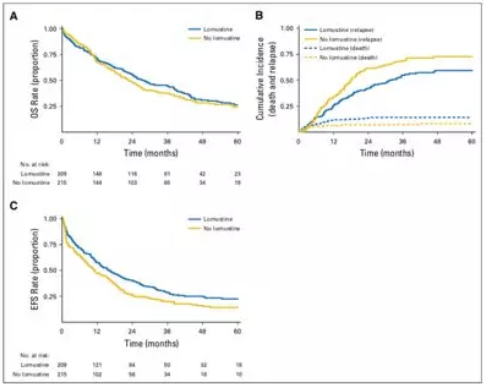
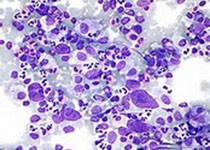
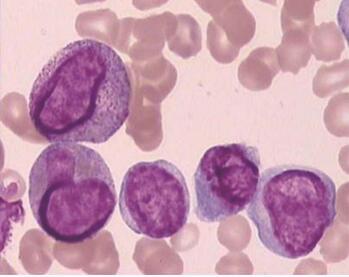
白血病是危害人类健康的重大疾病之一,治愈这类疾病最有效的手段是造血干细胞移植。本周,顶级期刊《科学》子刊上发表了一项重要成果,有望显着提高造血干细胞移植的成功率和安全性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#细胞移植#
32
#新发现#
29
#TRA#
17
#Transl#
26
好
72
#造血干细胞#
26
#造血#
27
#Med#
23