JAHA:淋巴B细胞水平可作为动脉粥样硬化预后的预测因子
2017-09-08 MedSci MedSci原创
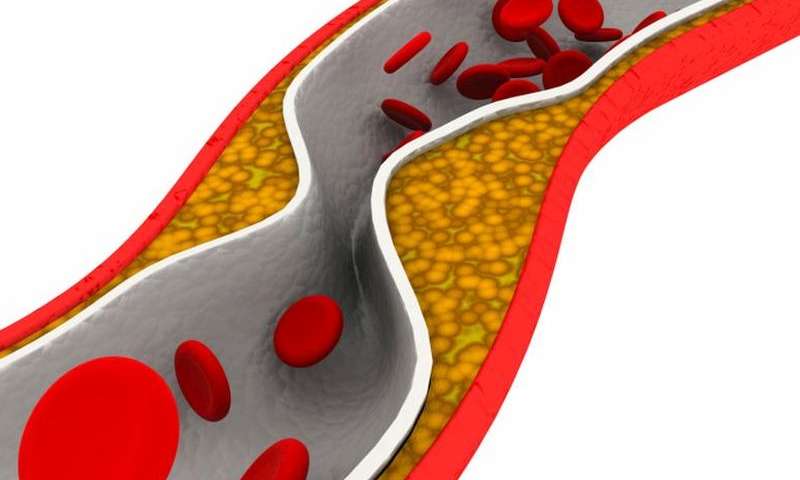
动脉粥样硬化是一种炎症性脂质紊乱的疾病,是急性缺血性事件的主要病理基础。尽管有许多小鼠模型研究表明淋巴B细胞与动脉粥样硬化相关,但在人上还未证实。本研究纳入了2009年至2011年168名拟行颈动脉内膜切除术的动脉粥样硬化患者,术前分离其外周血单个核细胞,液氮保存,经过温和外周血单核细胞融化后,对其不同的B细胞亚型包括记忆B细胞、CD27+CD43+ B1细胞等进行流式细胞分析。经过平均三年时间的
动脉粥样硬化是一种炎症性脂质紊乱的疾病,是急性缺血性事件的主要病理基础。尽管有许多小鼠模型研究表明淋巴B细胞与动脉粥样硬化相关,但在人上还未证实。本研究纳入了2009年至2011年168名拟行颈动脉内膜切除术的动脉粥样硬化患者,术前分离其外周血单个核细胞,液氮保存,经过温和外周血单核细胞融化后,对其不同的B细胞亚型包括记忆B细胞、CD27+CD43+ B1细胞等进行流式细胞分析。经过平均三年时间的随访,最终分析结果显示,人群的年龄为70.1±9.6岁,男性占62.8%,随访期间有54名患者出现过次要临床表现,大量的记忆B细胞水平与次要临床结局的保护呈相关性(HR, 0.30 [95% CI, 0.13-0.69]; P<0.01)。此外,高的激活后的记忆B细胞水平与次要临床结局的保护同样呈相关性(HR, 0.33 [95% CI, 0.14-0.77]; P=0.01)。研究结果表明,大量的记忆B细胞水平与颈动脉内膜切除术后的预后有关,淋巴B细胞水平可作为动脉粥样硬化患者临床预后的预测因子。原始出处:John A et al.High Levels of (Un)Switched
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










谢谢分享,学习了!
22
#粥样硬化#
20
不错的指南.为我们探讨研究提供了方针.必须给点个赞了!
60
#AHA#
26
#B细胞#
20
#预测因子#
27
继续学习中谢谢
53
学习了谢谢分享
62
动脉粥样硬化是一种炎症性脂质紊乱的疾病.是急性缺血性事件的主要病理基础.尽管有许多小鼠模型研究表明淋巴B细胞与动脉粥样硬化相关.但在人上还未证实.
65
研究结果表明.大量的记忆B细胞水平与颈动脉内膜切除术后的预后有关.淋巴B细胞水平可作为动脉粥样硬化患者临床预后的预测因子.
57