病例报告:一名患有肺动脉高压的男子出现双侧中央浆液性脉络膜病变样异常
2022-08-21 刘少飞 MedSci原创
在这项研究中,我们报告了一例PAH患者的双眼视力下降和变形,出现了中心性浆液性脉络膜病变(CSCR)样异常和视盘萎缩的病例。
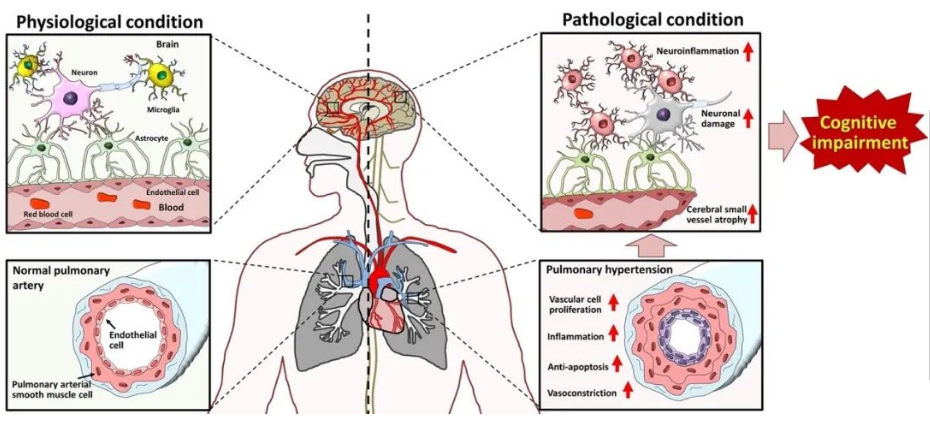
肺动脉高压(PAH)导致肺血管阻力逐渐增加,右心衰竭,如果不加以治疗会导致死亡。继发于PAH的眼部并发症则报道较少。在这项研究中,我们报告了一例PAH患者的双眼视力下降和变形,出现了中心性浆液性脉络膜病变(CSCR)样异常和视盘萎缩的病例。
病例:
主诉:
一名45岁的男子于2021年3月首次发现双眼中心视力下降、视力模糊和偏盲,1个月内病情恶化。
现病史:
他有PAH病史,于2015年6月被诊断为PAH,长期使用小剂量西地那非。他是一个人,没有兄弟姐妹,他的父母在大约10年前去世,没有记录PAH的家族史。
过去的病史:
他对PAH的药物治疗包括西地那非(2.5mg,bid)和安理申丹(5mg,qd)。他以前没有接受过类固醇治疗。
身体检查:
右眼BCVA为手指计数(FC)/10厘米,左眼为0.82(logMAR)。平均屈光不正为-3.25屈光度(右眼)和-1.00屈光度(左眼)。通过LENSTAR LS 900(HAAG-STREIT,美国)检测,他的轴长为23.49毫米(右眼)和22.46毫米(左眼)。眼压为19.9mmHg(右眼)和17.4mmHg(左眼)。裂隙灯生物显微镜检查发现,两只眼睛的巩膜和结膜血管都明显扩张和迂回(图1)。裂隙灯生物显微镜检查显示,除了两只眼睛的晶状体轻度混浊外,前节正常,没有虹膜炎的迹象。超声生物显微镜显示前房深度正常,即2.39毫米(右眼)和2.21毫米(左眼),并且前房角开放。
总结:一名45岁的男子出现了中心视力下降和双眼变形的症状。他有PAH病史和6年的低剂量口服西地那非治疗史。裂隙灯检查发现巩膜和结膜上的血管明显扩张和迂回。超视距彩色照片显示视网膜色素上皮的斑点和萎缩呈环状结构。超视场自体荧光显示视神经头和黄斑区周围有多个不规则的高自体荧光,呈星座状。光学相干断层扫描(OCTA)b扫描显示CSCR样改变。扫源光学相干断层扫描(SS-OCT)分析显示右眼视神经萎缩,杯/盘比例增大,这一点被围观者证实。荧光素血管造影(FA)显示黄斑和视神经头随着时间的推移有明显的渗漏,黄斑囊性水肿,在红外线和自体荧光的背景下显示早期阻断与后期染色的斑点,周边视网膜有轻微渗漏。吲哚青绿血管造影(ICGA)显示所有涡流静脉扩张、迂回和充血,没有明显渗漏。
结论:
治疗不足的PAH可能导致脉络膜充血并诱发CSCR样异常。
参考文献:
Zhou X, Zhang J, Gu L, Zhou H, Zhang J. Case report: Bilateral central serous chorioretinopathy-like abnormalities in a man with pulmonary arterial hypertension. Front Med (Lausanne). 2022 Aug 1;9:983548. doi: 10.3389/fmed.2022.983548. PMID: 35979218; PMCID: PMC9376321.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#脉络膜#
45
#动脉高压#
27
#病例报告#
44
#双侧#
39