Crit Care:重症监护病房中急性胆管炎患者特征分析
2021-02-06 MedSci原创 MedSci原创
在这项大型回顾性多中心研究中,研究人员发现AC相关死亡率随着时间推移显著降低。器官衰竭的严重程度、阻塞原因、AC局部并发症和胆道引流延迟超过48小时是导致死亡的危险因素。
目前,对于入住重症监护病房(ICU)的急性胆管炎(AC)患者结局和死亡的危险因素知之甚少。近日,危重病医学领域权威杂志Critical Care上针对这一问题发表了一篇研究文章。
这项多中心回顾性研究纳入了2005年至2018年期间入住11个重症监护病房的AC成年患者。研究人员采用多因素分析确定了住院死亡的危险因素。
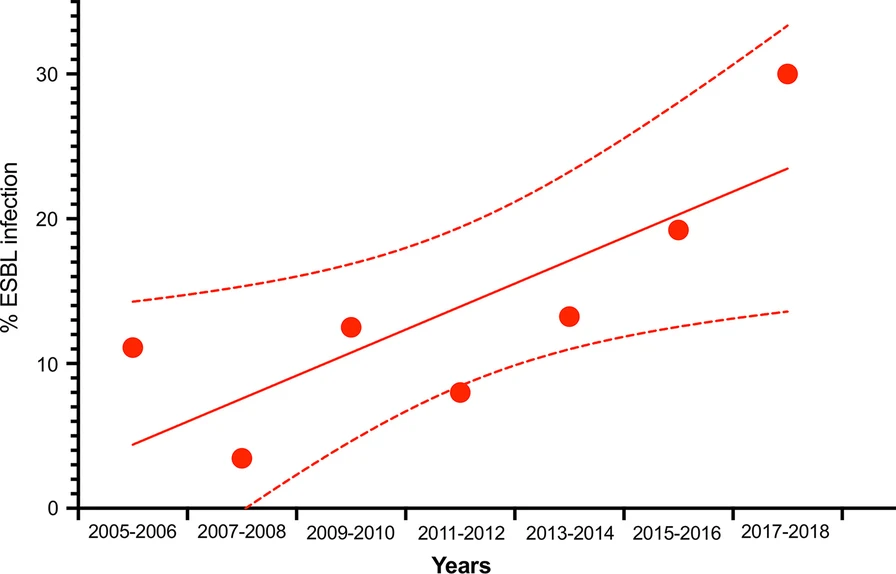
该研究共纳入了382例患者,院内死亡率为29%。患者入院时的SOFA评分为8 [5-11]。胆道阻塞主要与胆结石(53%)和癌症(22%)有关。总胆红素和PCT的中位数分别为83 µmol/L [50-147]和19.1 µg/L [5.3-54.8]。63%(n=252)的患者血液培养呈阳性,主要为革兰氏阴性杆菌(86%)和14%产生超广谱β-内酰胺酶的细菌。在入住ICU时,持续的梗阻很常见(79%),并且使用治疗性内镜逆行胰胆管造影术(76%)和经皮经肝胆道引流(21%)进行了胆道减压。调整后的死亡率随着时间的推移显著降低,调整后的年度死亡率OR为0.72 [0.54-0.96](p=0.02)。在多变量分析中,与院内死亡相关的入院因素为:SOFA评分(OR为1.14 [95%CI为1.05–1.24](p=0.001))、乳酸(OR为1.21 [95%CI为1.08–1.36],p<0.001)、总血清胆红素(OR为1.26 [95%CI为1.12-1.41],p<0.001),但与胆结石无关的梗阻(p<0.05)和AC并发症(OR为2.74 [95%CI为1.45-5.17],p=0.002)。从入住ICU到胆道减压之间的时间超过48小时与患者住院死亡率之间存在相关性(校正后OR为2.73 [95%CI为1.30-6.22],p=0.02)。
在这项大型回顾性多中心研究中,研究人员发现AC相关死亡率随着时间推移显著降低。器官衰竭的严重程度、阻塞原因、AC局部并发症和胆道引流延迟超过48小时是导致死亡的危险因素。
原始出处:
Jean-Rémi Lavillegrand.et al.Acute cholangitis in intensive care units: clinical, biological, microbiological spectrum and risk factors for mortality: a multicenter study.Critical Care.2021.https://ccforum.biomedcentral.com/articles/10.1186/s13054-021-03480-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#急性胆管炎#
34
#重症监护病房#
47
#监护#
41
#患者特征#
44
#胆管#
27
值得了解一下
77