J Clin Oncol:低剂量放疗联合顺铂可有效治疗HPV相关性口咽鳞癌
2021-02-01 MedSci原创 MedSci原创
降低放疗剂量可以提高高危型人乳头瘤病毒(HPV)相关口咽鳞癌(OPSCC)患者的生活质量(QOL)
降低放疗剂量可以提高高危型人乳头瘤病毒(HPV)相关口咽鳞癌(OPSCC)患者的生活质量(QOL)。但是,降低剂量的放射是否能产生与标准化疗相当的疾病控制和生活质量还没有得到证实。
这项随机的II期试验,招募了p16阳性、T1-T2 N1-N2b M0或T3 N0-N2b M0的OPSCC患者,且要求受试患者吸烟≤10包/年、在6周内接受了60Gy的强化放射治疗(IMRT)+顺铂(C)或5周60Gy的IMRT。要进入III期研究,治疗组的2年无进展存活率(PFS)必须高于历史控制率85%和1年平均MD Anderson吞咽困难指数(MDADI)的综合得分≥60。
治疗预后
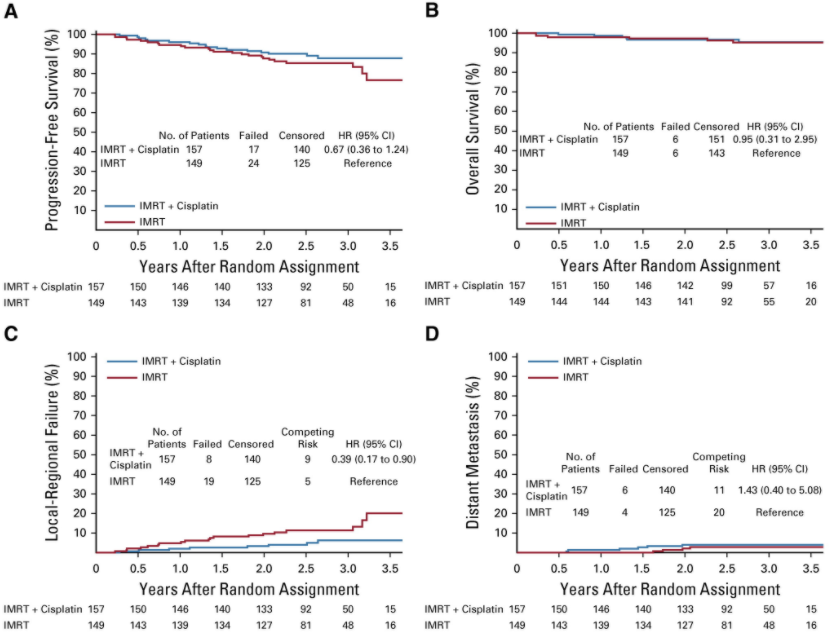
306例符合条件的患者被随机分至两组。强化放疗+化疗的两年生存率为90.5%,排除了2年生存率≤85%的无效假设(p=0.04)。强化放疗的2年无瘤生存率为87.6%(p=0.23)。IMRT+C组和IMRT组的1年MDADI得分分别为85.30分和81.76分。IMRT+C组和IMRT组的两年总生存率分别为96.7%和97.3%。
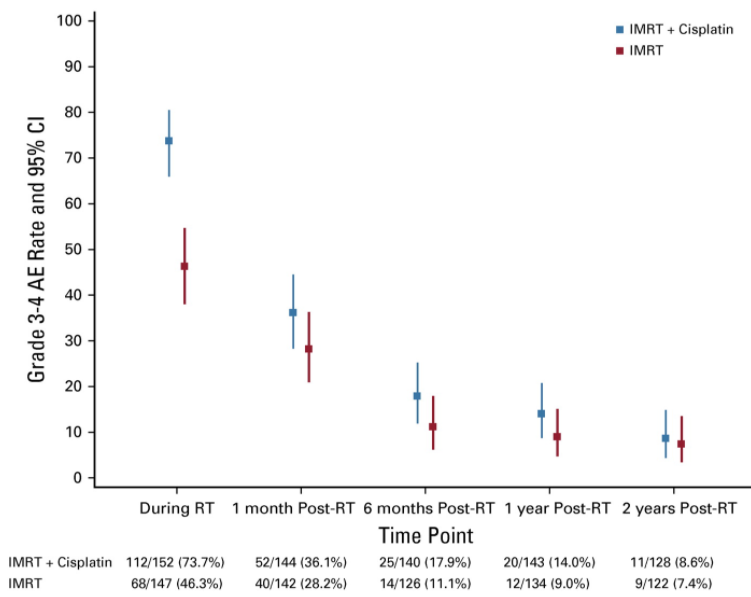
急性不良事件(AE)
急性不良事件(AE)定义为治疗结束后180天内发生的事件。IMRT+C组3-4级AE较多(79.6% vs 52.4%;p<0.001)。IMRT+C组和IMRT组的3-4级晚期AE发生率分别为21.3%和18.1%(p=0.56)。
综上,IMRT+C组达到了两个预定的终点,证明了可进入III期研究。值得注意的是,IMRT+C组的≥3级急性不良反应发生率较高。
原始出处:
Yom Sue S,Torres-Saavedra Pedro,Caudell Jimmy J et al. Reduced-Dose Radiation Therapy for HPV-Associated Oropharyngeal Carcinoma (NRG Oncology HN002). J Clin Oncol, 2021, undefined: JCO2003128.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Oncol#
25
#相关性#
20
#J Clin Oncol#点击查看更多该期刊内容
57
#铂#
22
#低剂量#
25
#鳞癌#
0
#低剂量放疗#
35
#有效治疗#
33
谢谢梅斯分享这么多精彩信息
39