JAMA Surg:新辅助放化疗联合手术可显著改善中国局部晚期食管鳞癌患者的长期预后
2021-06-28 MedSci原创 MedSci原创
新辅助放化疗联合手术可显著改善中国局部晚期食管鳞癌患者的长期预后
食管癌是世界第九大常见癌症,也是癌症相关死亡的第六大原因。超过50%的食管癌患者居住在东亚,其中90%的患者为食管鳞状细胞癌 (ESCC)。对于局部晚期食管癌患者,手术仍是目前的主要治疗手段。
局部晚期食管鳞状细胞癌(ESCC)患者手术后的预后仍然很差。新辅助放化疗 (NCRT) 已被证明有望提高患者生存率。与单纯手术相比,新辅助放化疗联合手术治疗能否提高局部晚期食管鳞状细胞癌 (ESCC) 患者的长期生存率?
本研究旨在对比NCRT联合手术与单纯手术治疗局部晚期ESCC患者的长期生存预后。
这是一项在中国的8家医疗中心开展的多中心、开放标签的随机3期临床试验,于2007年6月1日-2014年12月31日期间招募了451位18-70岁的胸段T1-4N1M0/T4N0M0期ESCC患者。患者随机接受NCRT+手术(NCRT组)或单纯手术(手术组)治疗。随访至2019年12月31日。主要终点是意向治疗人群的总生存率,次要终点是无病生存率。
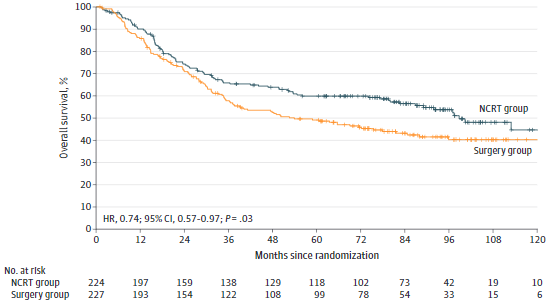
451位患者(平均 56.5岁,367位男性[81.4%])被随机分至两组:NCRT组 224位,手术组 227位,均被纳入意向治疗分析。截止2019年12月31日,共发生了224例死亡。
总生存率
中位随访53.5个月(四分位范围 18.2-87.4个月)。NCRT组患者的总生存期相比手术组患者的延长(风险比[HR] 0.74, 95%CI 0.57-0.97;p=0.03),5年总生存率分别是59.9% vs 49.1%。
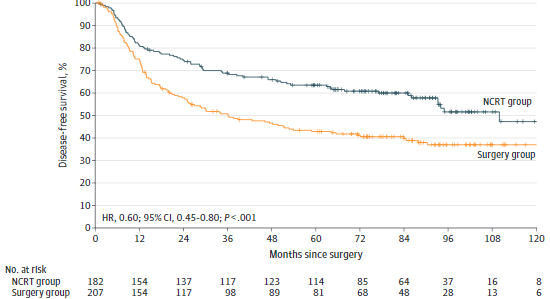
无病生存率
与手术组相比,NCRT组患者的无病生存期也明显延长(HR 0.60, 95%CI 0.45-0.80; p<0.01),5年无病生存率分别是63.6% vs 43.0%。
在这项随机临床试验中,NCRT联合手术治疗显著延长了考虑接受标准手术治疗的局部晚期ESCC患者的总生存率和无病生存率。
原始出处:
Yang Hong,Liu Hui,Chen Yuping et al. Long-term Efficacy of Neoadjuvant Chemoradiotherapy Plus Surgery for the Treatment of Locally Advanced Esophageal Squamous Cell Carcinoma: The NEOCRTEC5010 Randomized Clinical Trial.[J] .JAMA Surg, 2021, https://doi.org/10.1001/jamasurg.2021.2373
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#长期预后#
42
#鳞癌患者#
52
#辅助放化疗#
42
#局部晚期#
43
#新辅助#
41
特别好
72
#放化疗#
24
#局部#
36
#新辅助放化疗#
44
#食管#
28