CELL METAB:嗅觉缺失让你吃不胖
2017-07-06 海北 MedSci原创
个体全身能量的稳态调节取决于食物摄取和能量消耗之间的复杂平衡。这种平衡涉及了外周和中枢神经系统之间的协调反应,包括激素,多肽和神经递质。属于外周神经系统的嗅觉输入有助于协调人们对于食物的品鉴和选择,但是我们对它们在全身生理学和能量平衡中的作用还知之甚少。
个体全身能量的稳态调节取决于食物摄取和能量消耗之间的复杂平衡。这种平衡涉及了外周和中枢神经系统之间的协调反应,包括激素,多肽和神经递质。属于外周神经系统的嗅觉输入有助于协调人们对于食物的品鉴和选择,但是我们对它们在全身生理学和能量平衡中的作用还知之甚少。
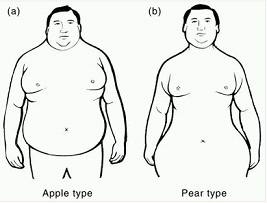
来自加州大学伯克利分校和德国马克斯普朗克代谢研究所的研究人员在细胞代谢杂志(Cell Metabolism)发文,他们发现,成熟嗅觉神经元被破坏的小鼠能够耐受饮食诱导的肥胖,并且伴随着棕色和腹股沟脂肪发热的增加。在肥胖症发生之后,嗅觉的急剧丧失也能够抑制体重的进一步增加,改善脂肪量以及胰岛素抵抗情况。减少的嗅觉输入能够刺激交感神经活动,促使白色和棕色脂肪细胞上β-肾上腺素能受体活化,促进脂肪分解。相反,如果消除小鼠成熟嗅觉神经元上的IGF-1受体,小鼠的嗅觉会更加灵敏,也会导致更严重的肥胖和胰岛素抵抗。
因此,研究人员的发现揭示了嗅觉系统在响应感觉和激素信号,控制能量稳态方面的新的双向功能。
原始出处:
Celine E. Riera et al. The Sense of Smell Impacts Metabolic Health and Obesity. Cell Metabolism. Volume 26, Issue 1, 5 July 2017, Pages 198–211.e5. DOI: https://doi.org/10.1016/j.cmet.2017.06.015
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Meta#
36
#Cell#
36
#CEL#
0
#MET#
37