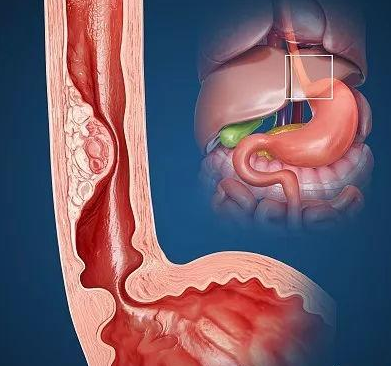
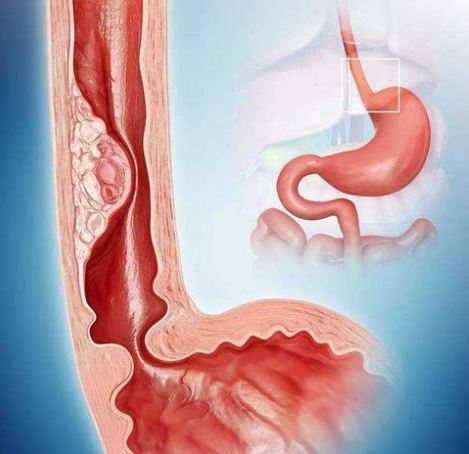
J Clin Oncol:EGFR抑制剂治疗EGFR扩增的胃食管交界癌的疗效
2022-04-13 Nebula MedSci原创
携带EGFR扩增变异的胃食管交界癌患者可从EGFR抑制剂治疗中获益
关于表皮生长因子受体抑制剂(EGFRi)的一项3期试验的亚分析结果显示,EGFRi可改善携带EGFR扩增的胃食管交界癌(GEA)患者的预后,但缺乏更大规模的分析数据。
本研究是一项多机构联合分析,旨在评估EGFRi在当下最大规模的携带EGFR扩增变异的GEA患者队列中的作用。
从6个国家的15家三级癌症中心筛查组织学明确诊断的、携带EGFR扩增变异的、转移性或不可切除的、接受EGFRi治疗的GEA患者。主要终点是客观缓解率。次要终点是无进展生存期和总生存期。
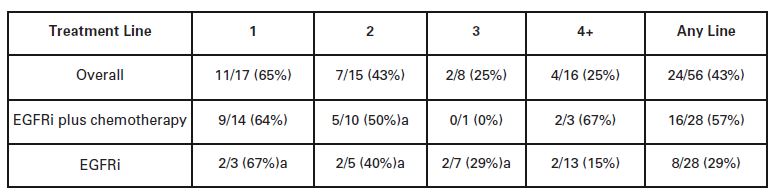
采用EGFRi作为不同线疗法的患者的客观缓解率
共筛查到60位接受EGFR治疗的符合纳入标准的患者,其中31位(52%)接受了同步化疗。中位随访了7.7个月,客观缓解率为43%,中位无进展生存期是4.6个月。
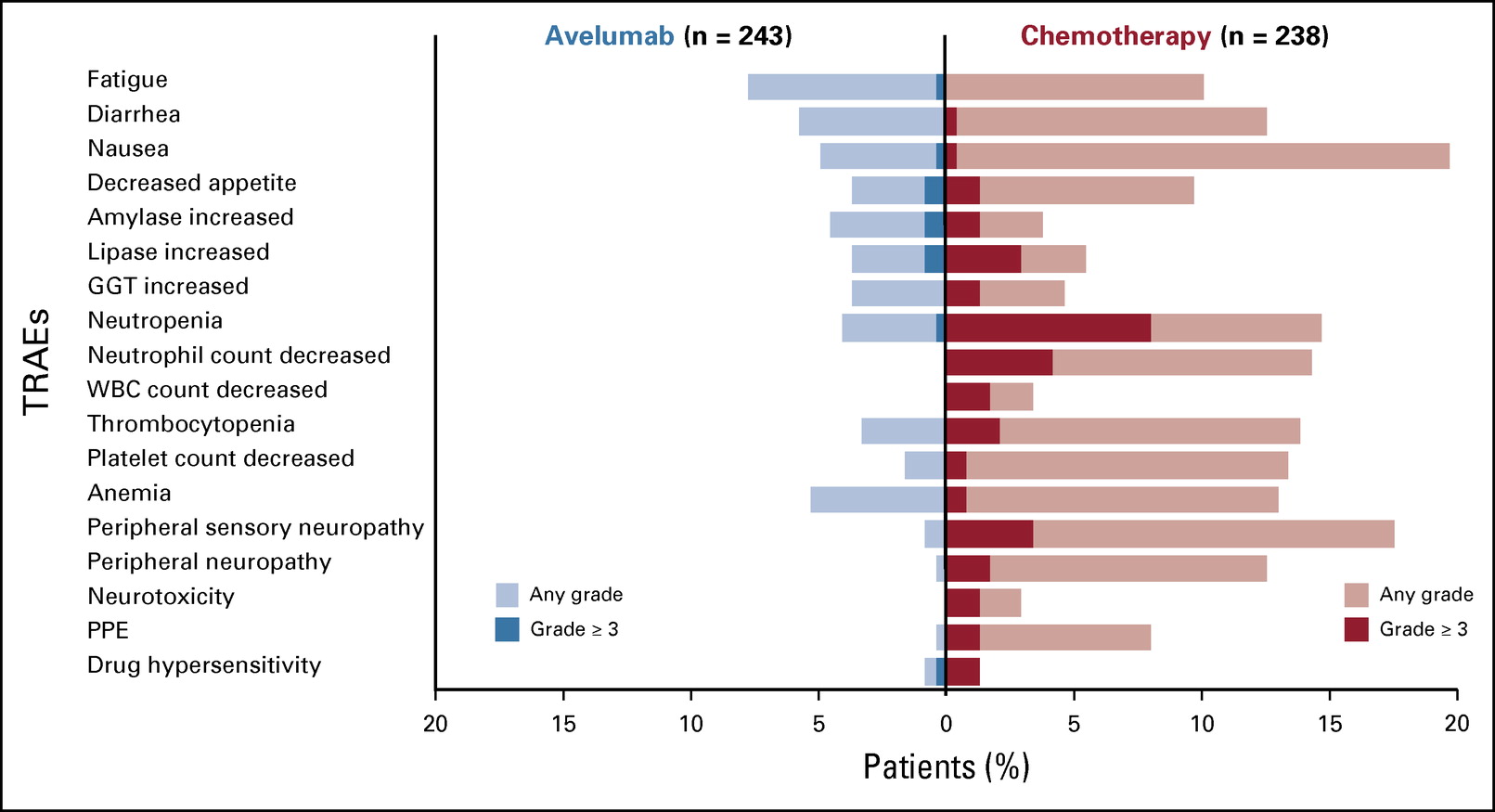
采用EGFRi作为不同线疗法的患者的总生存率和无进展生存率
采用EGFRi作为一线、二线或三线疗法的患者的中位总生存期分别是20.6个月、9个月和8.4个月。该生存期远远超过了临床基因组数据库(CGDB)中采用非-EGFRi作一线疗法的患者的中位总生存期(11.2个月)。但是,即使如此,对来自CGDB(2011年1月至2020年12月)的数据进行分析显示,只有5%的携带EGFR扩增的患者能从EGFRi治疗中获益。
总之,该研究结果显示,携带EGFR扩增变异的胃食管交界癌患者可从EGFR抑制剂治疗中获益。此外,一项关于EGFRi用于携带EGFR和/或MET扩增的GEA患者的前瞻性试验正在进行中。
原始出处:
Steven B. Maron, et al. Epidermal Growth Factor Receptor Inhibition in Epidermal Growth Factor Receptor–Amplified Gastroesophageal Cancer: Retrospective Global Experience. Journal of Clinical Oncology. March 29, 2022. https://ascopubs.org/doi/full/10.1200/JCO.21.02453.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#胃食管#
42
#抑制剂#
28
#Oncol#
0
#食管#
26
#GFR#
32
#胃食管交界癌#
40
感谢分享
37
好文章,值得一读。
35