AACR 2020:伯瑞替尼治疗MET异常NSCLC,ORR达30.5%
2020-04-29 找药宝典 找药宝典
伯瑞替尼治疗c-Met 异常的晚期非小细胞肺癌的I期临床试验结果公布这是一个开放性、多中心的I期临床研究,共纳入37例经治但未接受过c-Met抑制剂或HGF靶向治疗的局部晚期或转移性晚期NSCLC患者
伯瑞替尼治疗c-Met 异常的晚期非小细胞肺癌的I期临床试验结果公布这是一个开放性、多中心的I期临床研究,共纳入37例经治但未接受过c-Met抑制剂或HGF靶向治疗的局部晚期或转移性晚期NSCLC患者(NCT02896231)。研究分为剂量递增(19例)和剂量扩展(18例)两个阶段进行。 研究结果显示,8例患者仅检出c-MET过表达,11例仅携带Ex14跳读,8例仅检出MET基因扩增,另外10例患者检出不止一种MET变异。伯瑞替尼总体耐受性良好,未出现剂量限制性毒性。在所有可评估疗效的患者中(N=36),伯瑞替尼的ORR为30.5%(11/36) ,疾病控制率(DCR)为94.4% (34/36)。 亚组分析显示,c-MET过表达、扩增或Ex14跳跃突变的患者中,ORR 分别为30.6%, 41.2% 和 66.7%;在携带c-MET过表达且伴随基因扩增的患者(N=6)中的ORR为50%;在携带MET基因Ex14跳读且伴随基因扩增的患者(N=4)中,ORR达100%。 伯瑞替尼是中国第一个从大数据模拟、靶点验证到高通量筛选的精准治疗药物,该药物的临床试验获得了国家“十三五”重大新药创制专项资助。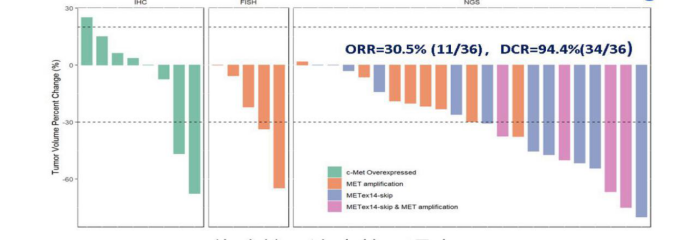
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#AACR 2020#
31
#MET#
28
#ACR#
18
#AACR#
24
#ORR#
31
#伯瑞替尼#
18
NSCLC下一步突破在于新靶点了,靶向治疗和免疫治疗基本见顶了,再有新的就需要新机制了
45