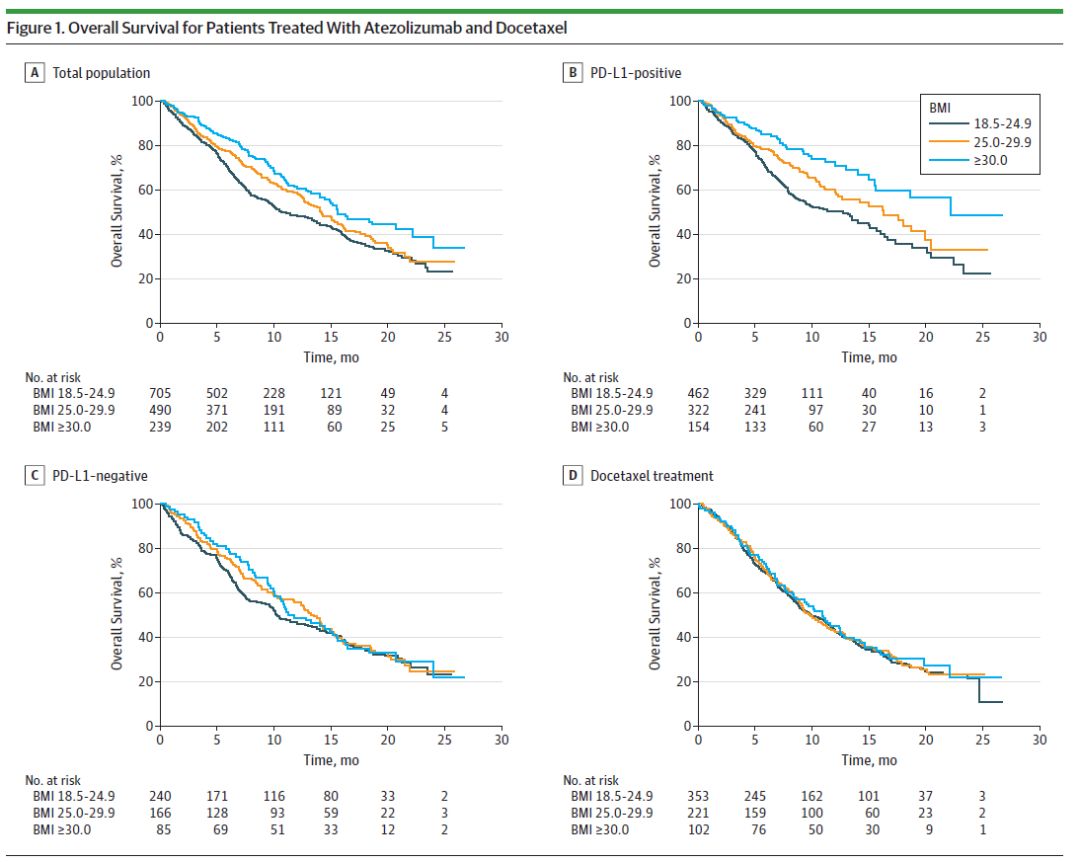
JAMA Oncol:PD-L1抗体对肥胖的癌症患者疗效更好
2019-12-27 曼话 医药魔方Pro
众所周知,肥胖是与癌症、糖尿病、心血管疾病以及其它疾病有关。全球癌症地图显示,体重超标(包括超重和肥胖)可增加患13种癌症的风险。不过肥胖患者患肿瘤以后的预后,确实有争议。在化疗时代,就有一些研究显示,肥胖患者往往然预后较偏瘦更好。原因可能与肥胖患者更能耐受化疗的副反应等原因有关。但是,免疫治疗时而代呢?12月26日,最新发表在JAMA Oncology上的一项研究却揭示,在某些情况下,BMI
众所周知,肥胖是与癌症、糖尿病、心血管疾病以及其它疾病有关。全球癌症地图显示,体重超标(包括超重和肥胖)可增加患13种癌症的风险。
不过肥胖患者患肿瘤以后的预后,确实有争议。在化疗时代,就有一些研究显示,肥胖患者往往然预后较偏瘦更好。原因可能与肥胖患者更能耐受化疗的副反应等原因有关。但是,免疫治疗时而代呢?12月26日,最新发表在JAMA Oncology上的一项研究却揭示,在某些情况下,BMI较高可能能够改善癌症患者的生存机会。
 图片来源:JAMA Oncology
图片来源:JAMA Oncology
具体来说,在该研究中,来自澳大利亚弗林德斯大学的Ganessan Kichenadasse博士及其同事聚焦了已被批准用于治疗非小细胞肺癌(NSCLC)的PD-L1抗体atezolizumab。他们惊讶地发现,BMI高的患者对atezolizumab的反应更强。BMI≥25的NSCLC患者接受该PD-L1抗体治疗后死亡率显著降低(尤其是在PD-L1高表达的情况下),明显获益于这类免疫检查点抑制剂。
 图片来源:Lancet Oncology
图片来源:Lancet Oncology
Kichenadasse博士之所以会想调查BMI与NSCLC患者对atezolizumab的响应的关联,是因为,2018年的一项回顾性研究报道, 在接受免疫检查点抑制剂和靶向疗法治疗的晚期黑色素瘤患者中,肥胖(BMI≥30)与总生存期(OS)、无进展生存期(PFS)改善有关,但在接受化疗治疗的患者中没有发现这种相关性。此外,2019年年初有研究[3]称,对于接受免疫检查点抑制剂治疗的晚期癌症患者,与BMI<25的患者相比,BMI≥25的超重或肥胖患者PFS和OS显著更长。
Kichenadasse博士领导的这项新研究汇总分析了涉及2261例NSCLC患者的4项国际多中心临床试验。其中两个是单臂II期试验:BIRCH(NCT02031458)和FIR(NCT01846416);两个是双臂随机试验,分别为II期试验POPLAR(NCT01903993)以及III期试验OAK(NCT02008227)。在POPLAR和OAK两个试验中,对照组患者接受每3周一次的多西紫杉醇治疗,直至病情进展或发生不可接受的毒性作用。在所有4项试验中,实验组患者都接受每3周一次的atezolizumab治疗。
Meta分析主要调查患者BMI与OS、PFS以及治疗相关不良事件的关系。
2261例患者中,有1548名参与者接受了atezolizumab治疗,排除40例BMI不可用的患者以及74例体重不足(BMI<18.5)的患者,剩余1434例患者可用于进一步分析。在这些患者中,705例(49%)患者体重正常、490例(34%)患者超重(25≤BMI<30),239例(7%)患者肥胖(BMI≥30)。
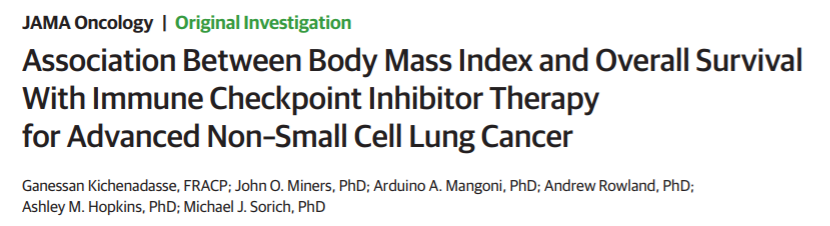
BMI与接受atezolizumab和多西紫杉醇治疗的患者OS和PFS之间的关系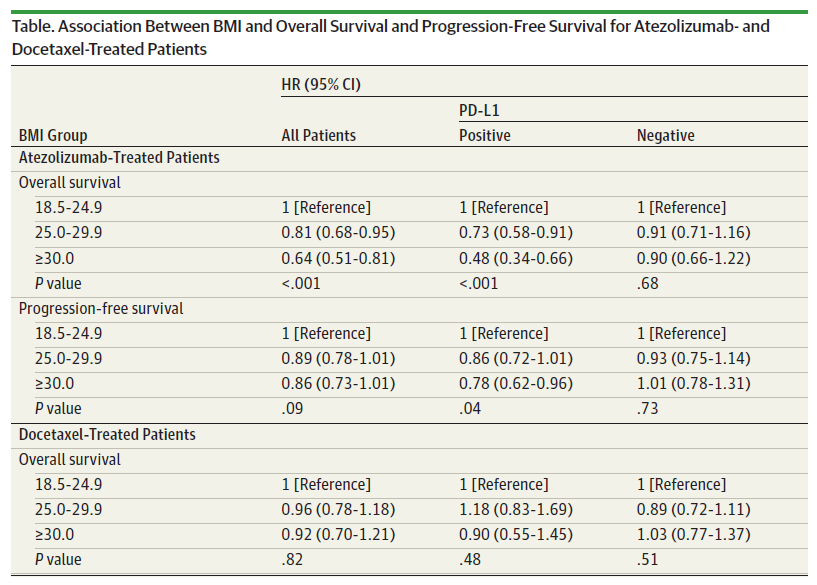 数据来源:JAMA Oncology
数据来源:JAMA Oncology
在接受atezolizumab治疗的患者中,BMI升高与OS之间存在线性关系。肥胖与接受atezolizumab治疗的患者的OS显著提高有关,但在接受多西紫杉醇治疗的患者中,肥胖与OS改善无关。在PD-L1高表达亚组中,BMI与OS/PFS的相关性最强。
接受atezolizumab和多西紫杉醇(Docetaxel)治疗的患者的OS(来源:JAMA Oncology)
此外,分析显示,治疗相关的不良事件与BMI无关。
总结来说,这项研究表明,较高的BMI似乎与接受atezolizumab治疗的NSCLC患者的OS改善有关。这增加了在未来的免疫检查点抑制剂试验中将基线BMI作为患者分层因素的可能性。
Kichenadasse博士说:“先前已有研究探索被称为‘肥胖悖论’的概念,即,虽然肥胖与患某种癌症的风险增加有关,但也能为某些患者带来更大的生存益处。而我们的研究提供了新的证据来支持这一假说,即高BMI和肥胖可能与患者对免疫治疗的反应有关。未来,我们需要进一步调查BMI与相关炎症之间的可能关联,这可能会帮助理解这种癌症治疗矛盾的反应背后的机制。”
原始出处:
[1] Ganessan Kichenadasse et al. Association Between Body Mass Index and Overall Survival With Immune Checkpoint InhibitorTherapy for Advanced Non–Small Cell Lung Cancer. JAMA Oncology(2019).
[2] Jennifer L McQuade et al. Associationof body-mass index and outcomes in patients with metastatic melanoma treated with targeted therapy, immunotherapy, or chemotherapy: a retrospective, multicohort analysis. Lancet Oncology(2018).
[3] Alessio Cortellini et al. A multicenter study of body mass index in cancer patients treated with anti-PD-1/PD-L1 immune checkpoint inhibitors: when overweight becomes favorable. Journal for ImmunoTherapy of Cancer(2019).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Oncol#
28
#PD-L1#
32
#癌症患者#
23
好
73
谢谢梅斯提供这么好的信息,学到很多
37
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
32
谢谢梅斯分享这么多精彩信息
46