J Clin Oncol:人源CD19 CAR T细胞可使复发或难治性B-ALL患者获得持久的缓解
2021-06-24 MedSci原创 MedSci原创
HuCART19用于复发或难治性B-ALL儿童和年轻成人患者可实现持久的缓解
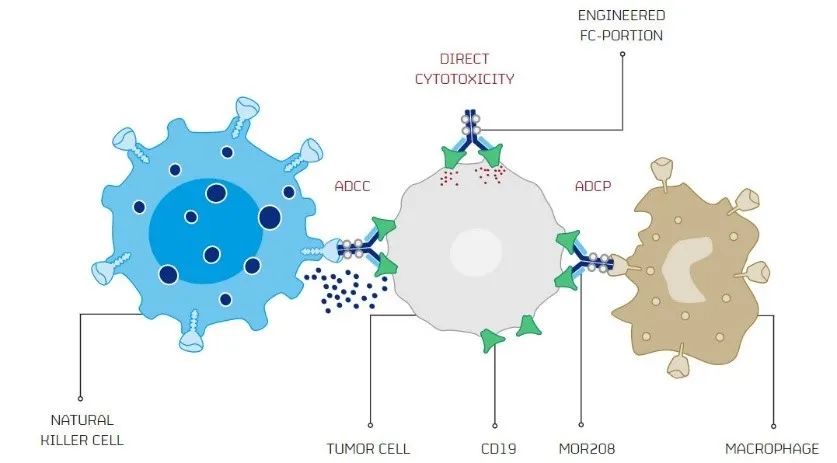
CD19靶向嵌合抗原受体 (CAR) 修饰的T细胞在急性B淋巴细胞白血病 (B-ALL) 中表现出前所未有的反应;但是,复发问题仍是一个重要的挑战。CAR T 细胞持续时间短是B-ALL复发的一个重要风险因素;因此,我们迫切需要提高CAR T细胞持久性的策略。
Myers等研究人员进行了一项飞行临床试验,招募了72例复发性/难治性B-ALL和2例复发性/难治性B细胞淋巴瘤儿童和年轻成年人患者,并根据既往有无接受过CAR治疗分成了两个队列:复治组(n=33)和CAR初治组(n=41),予以人源性CD19 CAR T细胞(huCART19)治疗。监测毒性、治疗反应和huCART19的持久性。
74位(1-29岁)患者都接受了huCART19治疗。62位(84%)患者发生了细胞因子释放综合征,其中5例(6.8%)为4级。29位(39%)患者报告了神经毒性,其中3例(4%)为3级或4级,全都得以治愈。
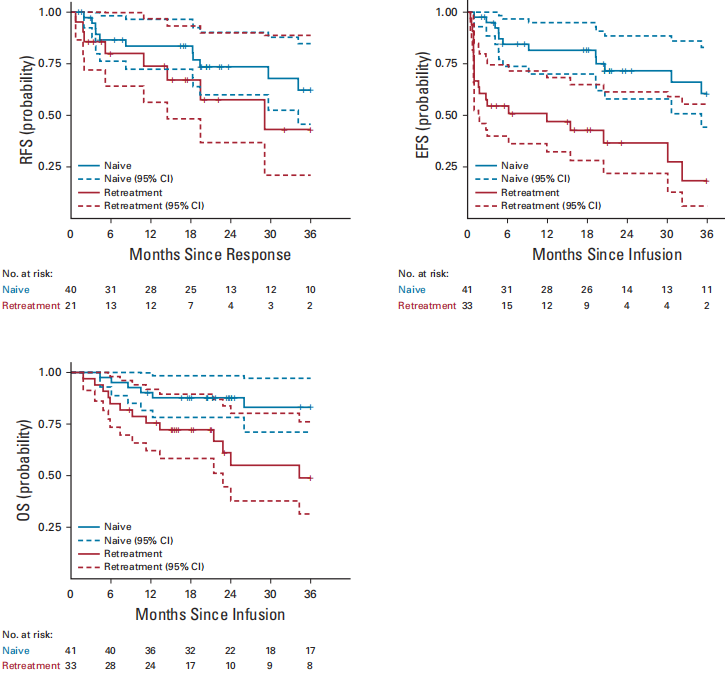
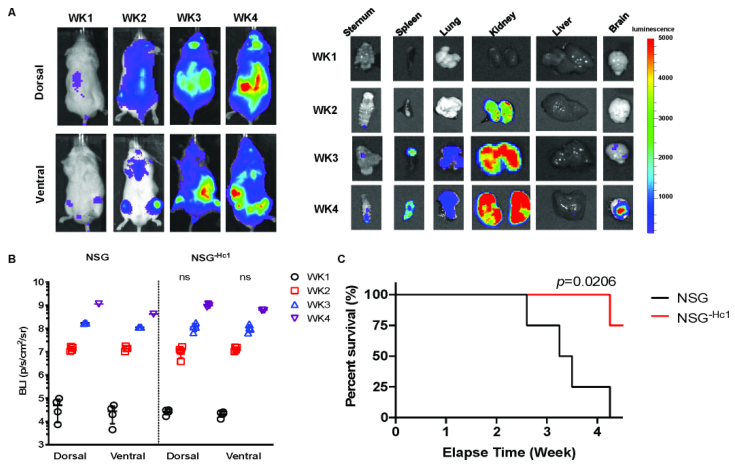
初治和复治患者的RFS、EFS和OS
在CAR初治队列中,输注huCART19一个月后的总反应率高达98%(在B-ALL患者中为100%);在复治队列中该反应率为64%。6个月时,CAR初治患者和复治患者huCART19持久性的丧失率分别为27%(95%CI 14-41)和48%(30-64),而B细胞的恢复率分别为15%(95%CI 6-20)和58%(33-77)。
CAR初治队列12个月和24个月时的无复发存活率分别为84%(95%CI 72-97)和74%(60-90);复治队列的12个月和24个月时的无复发存活率分别为74%(95%CI 56-97)和58%(37-90)。
综上所述,HuCART19用于复发或难治性B-ALL儿童和年轻成人患者可实现持久的缓解,包括既往CAR T 细胞治疗失败的患者。
原始出处:
Myers Regina M,Li Yimei,Barz Leahy Allison et al. Humanized CD19-Targeted Chimeric Antigen Receptor (CAR) T Cells in CAR-Naive and CAR-Exposed Children and Young Adults With Relapsed or Refractory Acute Lymphoblastic Leukemia.[J] .J Clin Oncol, 2021, undefined: JCO2003458. https://doi.org/10.1200/JCO.20.03458
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Oncol#
33
#ALL#
35
#CD19#
52
#B-ALL#
44
#难治性#
26
谢谢梅斯分享这么多精彩信息
44