EBMT 2020:LNP023治疗阵发性夜间血红蛋白尿(PNH)取得积极结果
2020-08-31 Allan MedSci原创
LNP023是一种针对PNH的口服型研究性药物。
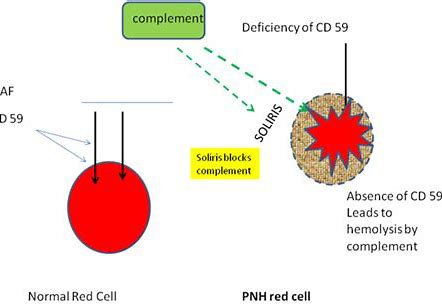
阵发性夜间血红蛋白尿症(PNH)是一种罕见、复杂且为后天造成的致命性血液疾病。患者身上部分造血骨髓的干细胞带有X染色体上PIG-A基因的突变,并且发生突变细胞的异常增生,导致该基因所转译的糖基脂酰肌醇锚定蛋白(GPI-anchored protein)有所缺损,而使红血球缺乏PIG-A酵素,致使CD55和CD59两种表面蛋白质缺失。
LNP023是一种针对PNH的口服型研究性药物。诺华公司今日公布了一项有关LNP023 II期临床试验(NCT03439839)的数据,结果表明,LNP023组患者发生积极溶血的几率降低,乳酸脱氢酶水平也显著降低,血管内溶血的生物标志物和血红蛋白(Hb)水平明显改善。与单独使用eculizumab相比,LNP023使Hb增加了2.87 g / dL(p <0.001)。
巴黎大学Peffault de Latour教授说:“这些新数据清楚地表明,LNP023可以控制这种疾病的溶血机制,并可能改变PNH的治疗方式”。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#BMT#
28
#阵发性夜间血红蛋白尿#
32
#PNH#
38
学习
75
学习了,涨知识了!
0