NEJM:艾伏尼布联合阿扎胞苷治疗IDH1突变AML的3期研究结果公布,患者获益显著
2022-04-22 MedSci原创 MedSci原创
急性髓系白血病(acute myelocytic leukemia,AML)包括所有非淋巴细胞来源的急性白血病。急性髓系白血病是造血系统的髓系原始细胞克隆性恶性增殖性疾病。是一个具有高度异质性的疾病群
急性髓系白血病(acute myelocytic leukemia,AML)包括所有非淋巴细胞来源的急性白血病。急性髓系白血病是造血系统的髓系原始细胞克隆性恶性增殖性疾病。是一个具有高度异质性的疾病群,它可以由正常髓系细胞分化发育过程中不同阶段的造血祖细胞恶性变转化。 AML是一种进展迅速的血液和骨髓癌症,是成人白血病中最常见的类型。在美国,每年约有20,000例新发病例。在中国,每年约有7.53万白血病新发病例,其中AML患者的占比约为59%。大多数AML患者最终会复发。复发或难治性AML患者的预后通常较差。患者五年生存率约29.5%。在被诊断为急性髓细胞白血病的患者中,约6~10%携带IDH1突变。 急性髓系白血病(AML)主要累及老年人(中位年龄68岁),老年患者和无法耐受强化诱导化疗的患者(所谓的unfit患者)可接受低强度的非治愈性方案(例如低剂量阿糖胞苷和去甲基化药物),而在unfit且突变状态未知的急性髓系白血病患者中,阿扎胞苷联合维奈托克可改善总生存期。然而,尽管取得了这一进展,unfit急性髓系白血病患者预后仍较差。 改善unfit的AML患者预后的策略之一,是使用新药靶向于参与白血病发生的分子学病灶。AML患者中有6~10%发生编码异柠檬酸脱氢酶1(IDH1)基因的体细胞突变,IDH1突变会催化D-2-羟基戊二酸生成,导致细胞代谢和表观遗传调控破坏,有助于肿瘤发生。多项研究表明,IDH1突变AML与高龄和预后较差相关,尤其是在核型正常的情况下。 艾伏尼布(Ivosidenib,拓舒沃)是IDH1突变的首创、口服、强效、靶向小分子抑制剂,一项纳入23例新诊断的IDH1突变急性髓系白血病患者的1b期试验的数据显示,艾伏尼布联合阿扎胞苷具有令人鼓舞的临床活性。艾伏尼布单药治疗(500 mg每日一次)已在美国获批单药治疗成人IDH1-突变型复发性或难治性急性髓性白血病,以及年龄≥75岁或患有无法使用强化诱导化疗的新诊断IDH1突变AML的成人患者。 近日,艾伏尼布联合阿扎胞苷治疗IDH1突变AML的3期AGILE研究的结果,研究结果发表在《新英格兰医学杂志》上。
这是一项全球、双盲、随机、安慰剂对照、3期研究,旨在评估艾伏尼布联合阿扎胞苷与安慰剂联合阿扎胞苷相比,在不适合强化诱导化疗的新诊断IDH1突变急性髓系白血病患者中的疗效和安全性。所有患者至少治疗6个周期,除非发生复发、疾病进展、不可接受的毒性作用或死亡。

患者纳入标准包括:年龄≥18岁,经美国食品药品监督管理局批准的Abbott RealTime IDH1体外聚合酶链反应(PCR)检测方法检测,中心确诊为既往未经治疗的IDH1突变急性髓系白血病;既往未接受过针对骨髓增生异常综合征的IDH1抑制剂或去甲基化药物治疗、ECOG体能状态评分为0-2分以及肝肾功能良好。不适合接受强化化疗的定义为年龄≥75岁或至少具有以下一种医学状况:ECOG体能状态评分为2,重度心脏疾病(例如需要治疗的充血性心力衰竭、左心室射血分数≤50%或慢性稳定型心绞痛),重度肺部疾病(例如肺一氧化碳弥散量≤65%或1秒用力呼气量≤65%)、肌酐清除率低于45 mL/min或胆红素水平高于正常范围上限的1.5倍。
主要终点为EFS。次要终点包括CR、OS、CR伴不完全血液学缓解、ORR、安全性和健康相关生活质量。
患者于2018年3月至2021年5月入组,截至2021年3月18日(数据截止),在筛选的295例患者中,146例接受了随机(图1),其中72例分配至艾伏尼布+阿扎胞苷组(中位年龄76.0岁),74例分配至安慰剂+阿扎胞苷组(中位年龄75.5岁)。
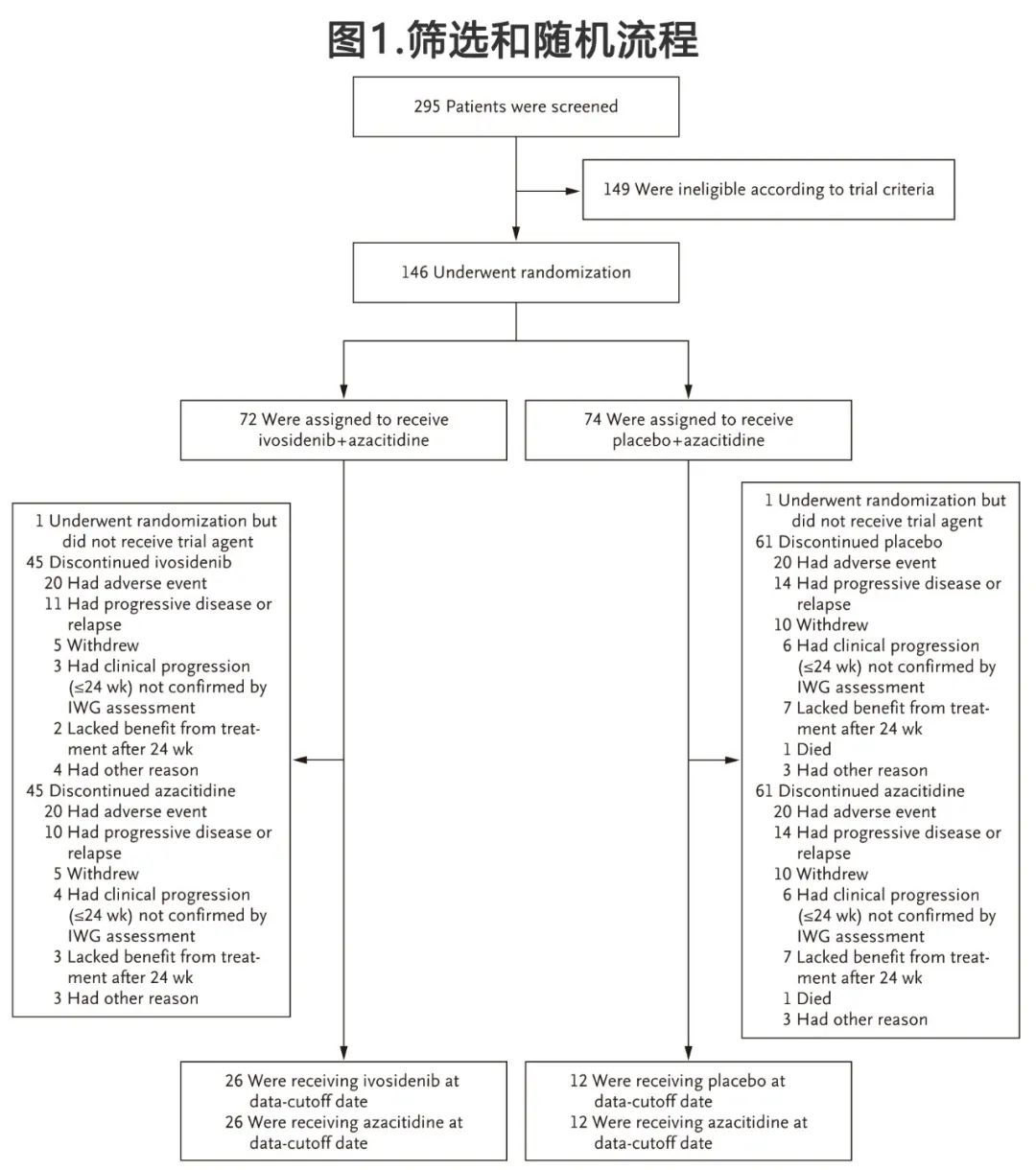
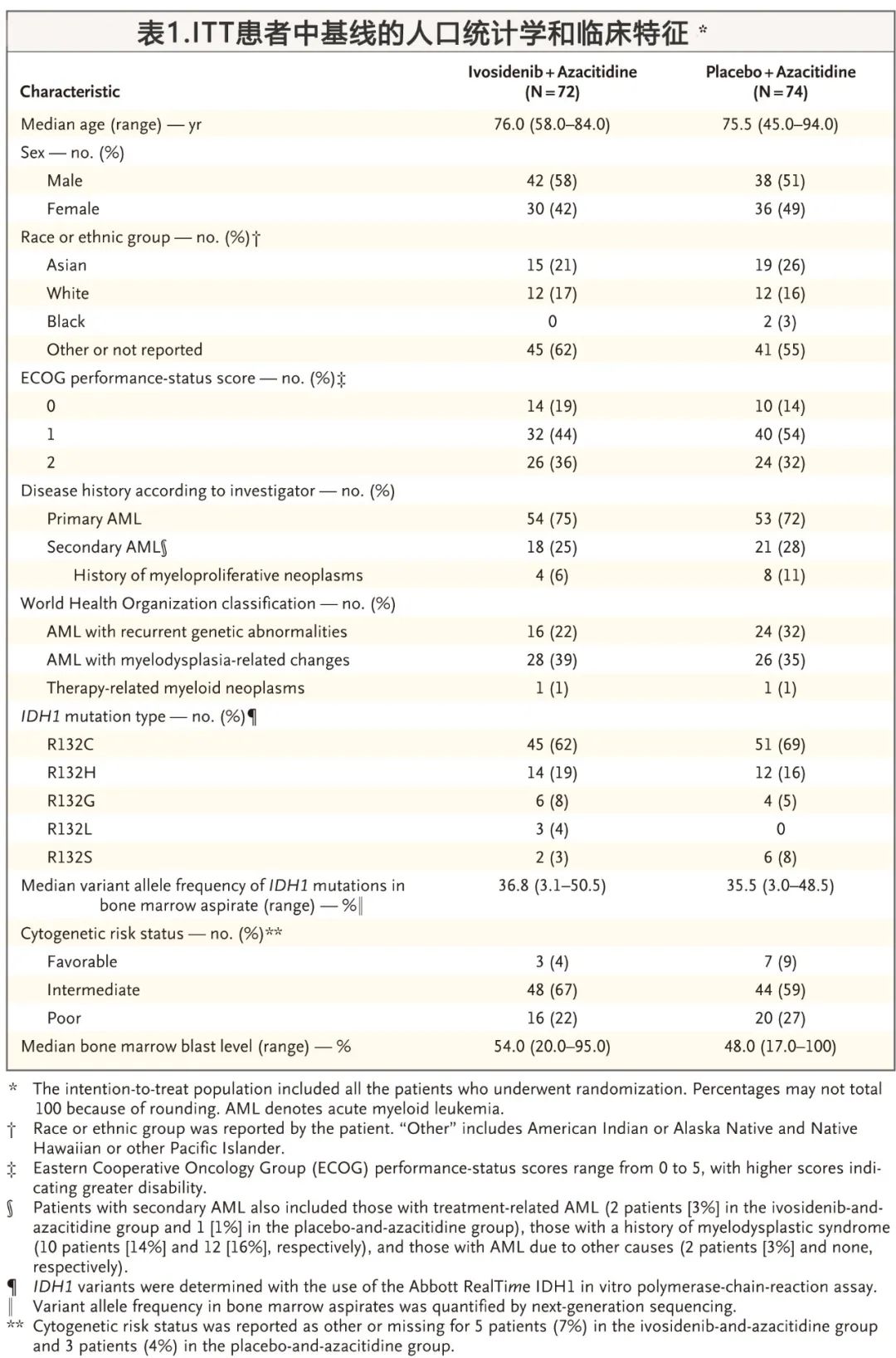
两个试验组患者基线人口统计学和临床特征相似(表1)艾伏尼布+阿扎胞苷组54例(75%)为原发性急性髓系白血病,18例(25%)为继发性急性髓系白血病;安慰剂+阿扎胞苷组53例(72%)为原发性急性髓系白血病,21例(28%)为继发性急性髓系白血病。与安慰剂+阿扎胞苷组20例(27%)相比,艾伏尼布+阿扎胞苷组共有16例(22%)患者为细胞遗传学低危。在数据截止,共有39例患者持续接受治疗(艾伏尼布+阿扎胞苷组27例[38%],安慰剂+阿扎胞苷组为12例[16%])。
主要疗效终点
无时间生存期定义为:从随机化到治疗失败(24周未达到CR)、缓解后复发或任何原因的死亡,先到为准。
中位随访12.4个月。艾伏尼布+阿扎胞苷组的无事件生存期显著长于安慰剂+阿扎胞苷组(治疗失败、缓解后复发或死亡的风险比为0.33;95%置信区间[CI],0.16~0.69;P= 0.002)(图2A)。由于两组均有超过一半的患者在第24周时未达到完全缓解,因此两组的中位EFS相同(均为0.03个月);但与安慰剂+阿扎胞苷组6个月时无事件率20%和12个月时无事件率12%相比,艾伏尼布+阿扎胞苷组6个月时估计无事件率为40%,12个月时估计无事件率为37%。各亚组的EFS获益见图2C。
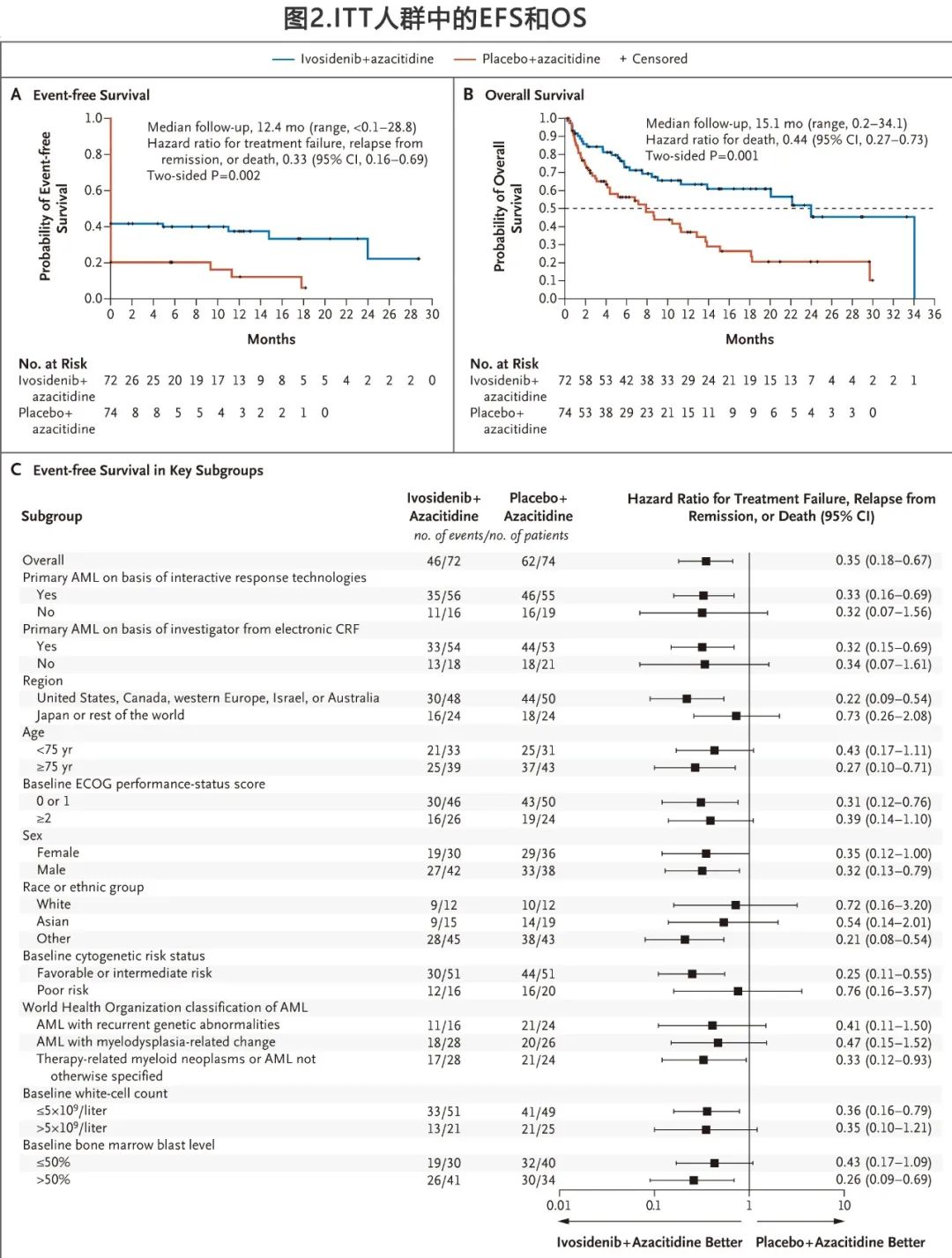
24周时艾伏尼布+阿扎胞苷组CR率为38%,而安慰剂+阿扎胞苷组为11%;且24周CR患者的无事件生存期也有利于艾伏尼布+阿扎胞苷组。作者还对无事件生存期进行了敏感性分析,治疗失败定义为治疗至少24周后缺乏完全缓解、完全缓解伴不完全血液学恢复或骨髓中白血病细胞形态学清除;根据该定义艾伏尼布+阿扎胞苷组中位无事件生存期为22.9个月,而安慰剂+和阿扎胞苷组为4.1个月。
次要终点
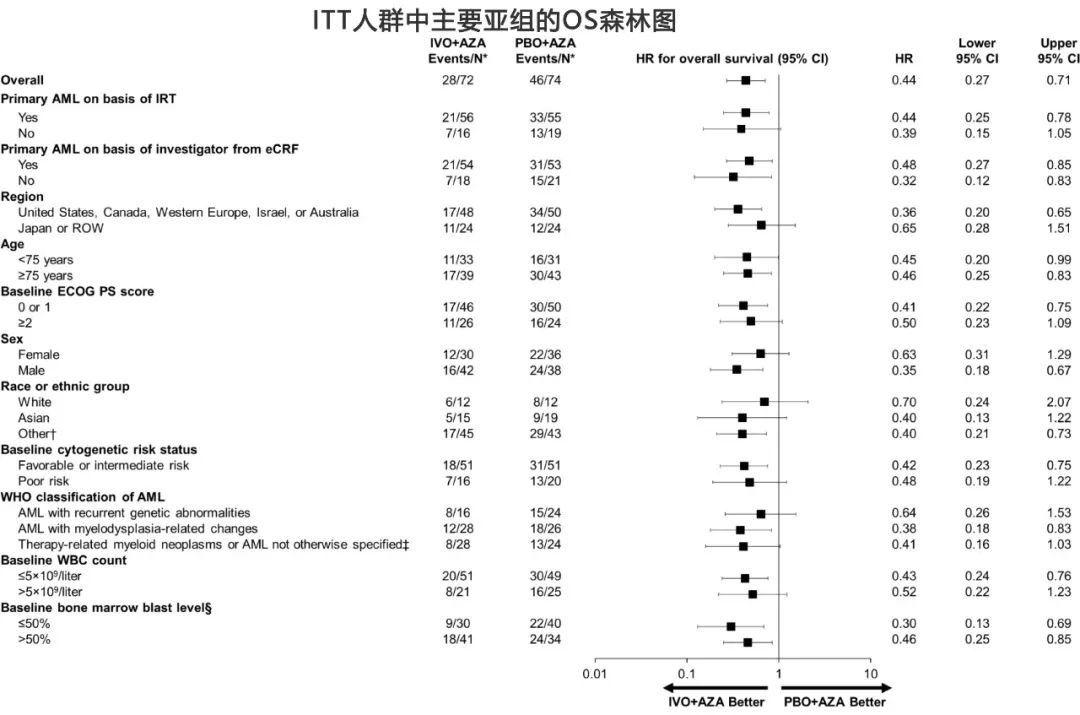
共74例死亡(艾伏尼布+阿扎胞苷组28例[39%],安慰剂+阿扎胞苷组46例[62%]),中位OS分别为24.0个月和7.9个月(死亡风险比0.44;95%CI,0.27~0.73;P= 0.001)(图2B)。各亚组的OS获益见下图。
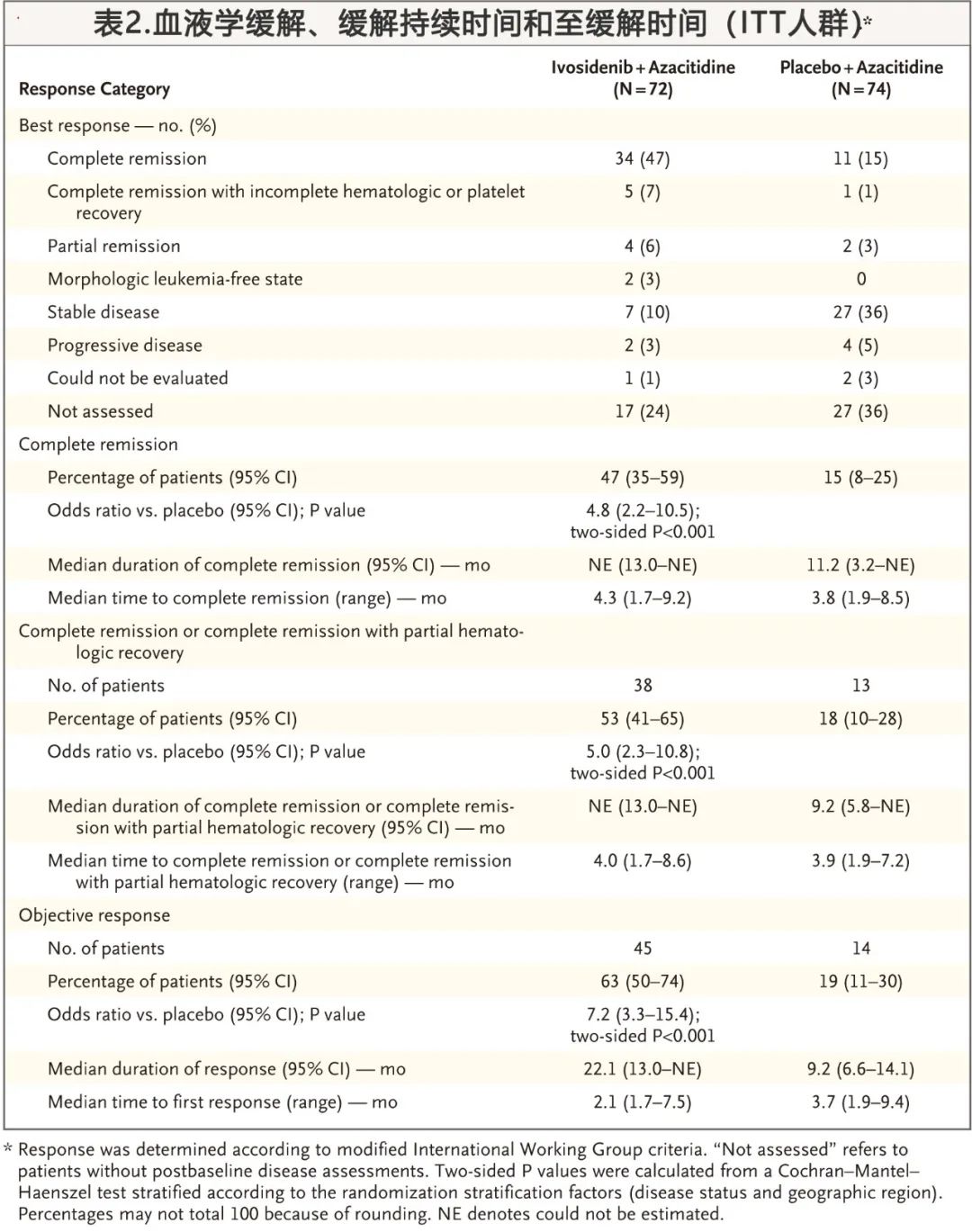
血液学缓解、缓解持续时间和至缓解时间见表2。72例患者中,艾伏尼布+阿扎胞苷组34例患者(47%)和安慰剂+阿扎胞苷组74例患者中11例患者(15%)获得CR (P < 0.001);前者中位CR缓解持续时间,而安慰剂+阿扎胞苷组为11.2个月。在完全缓解的患者中,艾伏尼布+阿扎胞苷组患者在12个月时保持完全缓解的估计概率为88%,而安慰剂+阿扎胞苷组为36%。艾伏尼布+阿扎胞苷组中位至CR时间为4.3个月,安慰剂+阿扎胞苷组为3.8个月。艾伏尼布+阿扎胞苷组有38例(53%)达到完全缓解/完全缓解伴部分血液学恢复,而安慰剂+阿扎胞苷组为13例(18%) (P< 0.001)。两组的ORR分别为62%和19% (P < 0.001),中位DOR分别为22.1个月和9.2个月;中位治疗持续时间为6.0个月和2.8个月。
血液学改善
在基线时存在红细胞和/或血小板输血依赖的患者中,与安慰剂和阿扎胞苷(18%)相比,艾伏尼布+阿扎胞苷组(46%)组转变为非输血依赖的比例更高(P= 0.006)。
转化结果
基线时骨髓穿刺液中IDH1突变的中位变异等位基因频率,艾伏尼布+阿扎胞苷组为36.8%,安慰剂+阿扎胞苷为35.5%,IDH1突变的变异等位基因频率无法预测两组的缓解情况。
在样本可用的120例患者(艾伏尼布+阿扎胞苷组58例,安慰剂+阿扎胞苷62例)中,患者均携带另一个基因的至少一个突变,其中DNMT3A、SRSF2和RUNX1是两组中最常见的,在其他感兴趣的突变中,包括RTK通路突变(FLT3、KIT、KRAS、NRAS和PTPN11)和TP53,艾伏尼布+阿扎胞苷组比安慰剂+阿扎胞苷CR率更高。
在骨髓单核细胞中评估了IDH1突变清除率,定义为治疗期间一个或多个时间点未检测到IDH1突变。在可获得样本的完全缓解/完全缓解伴部分血液学恢复的患者中,艾伏尼布+阿扎胞苷组33例患者中有17例(52%)的IDH1突变清除,而安慰剂+阿扎胞苷组10例患者中有3例(30%)的IDH1突变清除。在有骨髓单个核细胞IDH1突变清除数据的患者中,艾伏尼布+阿扎胞苷组14/43 例(33%)为 IDH1突变清除伴完全缓解,相比之下,安慰剂+阿扎胞苷组为2/31例(6%) (P= 0.009)。
生活质量
在所有生活质量EORTC QLQ-C30子量表中,结果均有利于艾伏尼布+阿扎胞苷组。两组中初始生活质量的下降与至缓解时间一致,但从第5周期至第19周期,大多数子量表显示,艾伏尼布+阿扎胞苷组的健康相关生活质量与基线相似或较基线改善,而安慰剂和阿扎胞苷组均未发生较基线改善。
安全性
常见不良事件总结见表3,艾伏尼布+阿扎胞苷组共有66/71例(93%)发生≥3级不良事件,安慰剂+阿扎胞苷组共有69/73例(95%)发生≥3级不良事件。两组中发生比例超过15%的≥3级不良事件包括:发热性中性粒细胞减少(艾伏尼布+阿扎胞苷组为28%,安慰剂+阿扎胞苷组为34%)、贫血(分别为25%和26%)、中性粒细胞减少(分别为27%和16%)、血小板减少(分别为24%和21%)和肺炎(分别为23%和29%)。
艾伏尼布+阿扎胞苷组患者中,发生任何级别感染的患者百分比为28%,而安慰剂+阿扎胞苷组为49%;且随着时间的推移,仅艾伏尼布+阿扎胞苷组观察到中性粒细胞绝对计数较基线增加,特别是在第一个周期。
艾伏尼布+阿扎胞苷组出血事件发生率高于安慰剂+阿扎胞苷组(41% vs. 29%);前者发生任何级别分化综合征(differentiation syndrome)的患者百分比为14%(无≥4级事件),安慰剂+阿扎胞苷组为8%(包括1例4级事件),所有病例均给予糖皮质激素、利尿剂、羟基脲等处理;艾伏尼布+阿扎胞苷组至任何级别分化综合征的中位时间为19.5天。两组均未观察到因分化综合征导致的死亡。
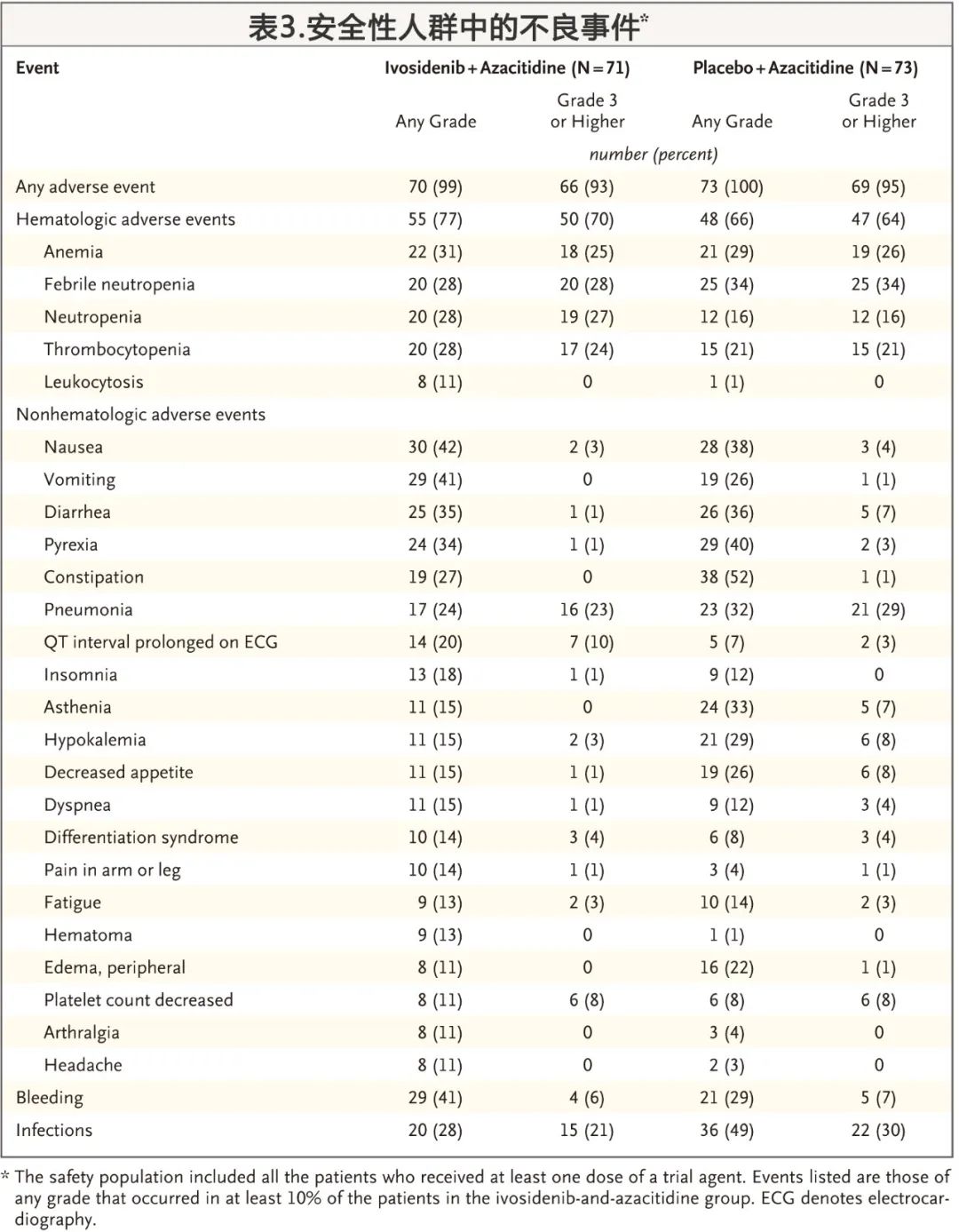
两组均有19例患者发生导致两种试验药物停药的不良事件:最常见的是艾伏尼布+阿扎胞苷组的肺栓塞(2例[3%])和安慰剂+阿扎胞苷组的肺炎(4例[5%])。仅艾伏尼布+阿扎胞苷组的4例患者(6%)发生导致两种试验药物剂量降低的不良事件。
艾伏尼布或安慰剂的中位相对剂量强度,在艾伏尼布+阿扎胞苷组为98.4%,安慰剂+阿扎胞苷组为97.7%;阿扎胞苷的中位相对剂量强度,分别为92.5%和95.2%。
艾伏尼布+阿扎胞苷组37例(52%)以及安慰剂+阿扎胞苷组28例(38%)发生导致两种试验药物均中断的不良事件,导致给药中断的最常见不良事件包括中性粒细胞减少(艾伏尼布+阿扎胞苷组23%,安慰剂+阿扎胞苷组4%)、发热性中性粒细胞减少(分别为10%和8%)和感染性肺炎(8%和7%)。艾伏尼布+阿扎胞苷组0例(14%)患者和安慰剂+阿扎胞苷组21例(29%)死于不良事件。
这项3期研究表明,艾伏尼布联合阿扎胞苷治疗与两者单独治疗急性白血病的不良事件相似,能有效延长无事件生存期,增加完全缓解,以及延长老年或其他不适合诱导化疗的IDH1突变急性髓系白血病患者的OS。在接受艾伏尼布联合阿扎胞苷治疗的患者中发生了持久而深入的缓解,且IDH1突变多清除,这一发现强调了靶向突变IDH1蛋白的益处。安全性方面,总体而言艾伏尼布联合阿扎胞苷很少因毒性作用而停止治疗。
基石药业首席医学官杨建新博士表示:“我们非常高兴地看到AGILE III期AML研究优异数据在《新英格兰医学杂志》发表,这充分彰显了全球权威学术期刊对该研究结果和学术价值的高度认可。IDH1突变AML患者的预后差,尤其是IDH1突变的未经强化化疗的初治AML患者。拓舒沃®联合阿扎胞苷疗法将有望为这部分患者带来新的治疗选择。我们计划与中国国家药品监督管理局(NMPA)展开沟通,期待尽快将这一创新疗法带给更多中国患者。”
关于AGILE III期AML研究 (NCT03173248)
AGILE研究是一项全球III期、多中心、双盲、随机、安慰剂对照临床试验,旨在评估艾伏尼布联合阿扎胞苷与安慰剂联合阿扎胞苷,在不符合强烈化疗条件的新诊断AML患者中的疗效和安全性。该研究的主要终点是EFS,定义为从随机到治疗失败、缓解后复发或任何原因引起的死亡(以先发生者为准)的时间。治疗失败的定义为直到第24周患者仍未能达到CR。
关键次要终点包括: CR率,定义为达到CR的受试者比例; OS,定义为从随机日期到任何原因的死亡日期的时间;CR和CR伴部分血液学恢复的缓解(CRh)率,定义为达到CR或CRh的受试者比例;ORR,定义为达到CR、CR伴不完全血液学恢复(CRi/CRp)、部分缓解(PR)或形态学无白血病状态(MLFS)的受试者比例。
关于急性髓系白血病(AML)
急性髓系白血病(AML)是一种进展迅速的血液和骨髓癌症,是成人白血病中最常见的类型。在美国,每年约有2万新发病例,欧洲每年新增4.3万例。[1,2,7]在中国,每年约有7.53万白血病新发病例,其中AML患者的占比约为59%。AML的发病率随着年龄的增长而显著增加,诊断的中位年龄约为68岁。[1]大多数患者对化疗无反应会进展成复发或难治性AML[3],患者五年生存率约29.5%。[1]对于6~10%AML的患者,IDH1酶突变会阻断正常的血液干细胞分化,从而导致急性白血病的发生。[4]
关于拓舒沃®(艾伏尼布片)
拓舒沃®是一种针对IDH1突变酶的口服靶向抑制剂。拓舒沃® 已经获得中国国家药品监督管理局(NMPA)批准,用于治疗携带IDH1易感突变的成人复发或难治性急性髓系白血病(R/R AML)患者。
2020年,拓舒沃被中国国家药品监督管理局药品审评中心纳入“临床急需境外新药名单(第三批)”,获得快速通道审评审批资格。同时,作为全球同类首创的强效、高选择性口服IDH1抑制剂,拓舒沃以其明确的临床优势,入选了2020版《CSCO恶性血液病诊疗指南》。
拓舒沃®获美国食品药品监督管理局(FDA)批准,用于单药治疗经FDA批准的检测方法确诊的携带IDH1易感突变的成人复发或难治性急性髓系白血病患者,以及年龄≥75岁或因为其它合并症无法使用强化化疗的携带IDH1易感突变的新诊断AML成人患者。2021年,拓舒沃®获批准作为首个且唯一的靶向疗法,用于治疗经FDA批准的检测方法确诊的先前经过治疗的IDH1突变的局部晚期或转移性胆管癌患者。
美国FDA先后授予拓舒沃®联合阿扎胞苷方案“突破性疗法”认定,用于治疗新诊断的年龄至少75岁或因其它合并症而无法使用强化化疗的携带IDH1易感突变的AML成人患者,以及艾伏尼布“突破性疗法”认定,用于治疗携带IDH1易感突变的复发/难治性骨髓增生异常综合征的成人患者(MDS)。
关于基石药业
基石药业(香港联交所代码: 2616)是一家生物制药公司,专注于研究开发及商业化创新肿瘤免疫治疗及精准治疗药物,以满足中国和全球癌症患者的殷切医疗需求。成立于2015年底,基石药业已集结了一支在新药研发、临床研究以及商业运营方面拥有丰富经验的世界级管理团队。公司以肿瘤免疫治疗联合疗法为核心,建立了一条15种肿瘤候选药物组成的丰富产品管线。目前,基石药业已经获得了四款创新药的七个新药上市申请的批准。多款后期候选药物正处于关键性临床试验或注册阶段。基石药业的愿景是成为享誉全球的生物制药公司,引领攻克癌症之路。
参考文献
Pau Montesinos,et al.Ivosidenib and Azacitidine in IDH1-Mutated Acute Myeloid Leukemia.N Engl J Med . 2022 Apr 21;386(16):1519-1531. doi: 10.1056/NEJMoa2117344.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#IDH1#
60
#结果公布#
50
#研究结果#
57
#阿扎胞苷#
81
#IDH1突变#
40
NEJM上果然牛,感谢梅斯更新及时
39
#肿瘤#
76
#学习#
80
#学习#
76