Opdivo联合Yervoy显著延长胸膜间皮瘤患者存活率!
2020-08-10 Allan MedSci原创
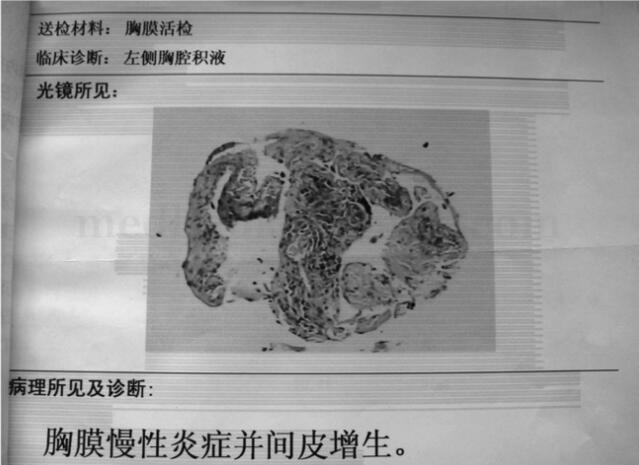
恶性胸膜间皮瘤(MPM)是一种罕见肿瘤,通常起源于胸膜腔的间皮表面。间皮瘤也可能起源于腹膜表面、睾丸鞘膜或心包。MPM的预后较差,患者的中位生存期为6-18个月。
恶性胸膜间皮瘤(MPM)是一种罕见肿瘤,通常起源于胸膜腔的间皮表面。间皮瘤也可能起源于腹膜表面、睾丸鞘膜或心包。MPM的预后较差,患者的中位生存期为6-18个月。
近期研究表明,免疫疗法Opdivo(nivolumab)联合Yervoy(ipilimumab)改善了先前未经治疗的恶性胸膜间皮瘤(MPM)患者的生存率。在III期CheckMate-743试验中,Opdivo联合Yervoy降低了26%的死亡风险,中位总体生存期为18.1个月,而基于铂的标准疗法的中位总体生存期为14.1个月。经过两年的随访,接受Opdivo联合Yervoy组合治疗的患者中有41%存活,而接受化疗的患者中有27%存活。
在间皮瘤中,患有非上皮样癌的患者通常预后较差。CheckMate-743试验表明,Opdivo联合Yervoy显著改善了非上皮样和上皮样MPM患者的生存率。

荷兰癌症研究所和莱顿大学胸腔肿瘤学系的Paul Baas博士说:“恶性胸膜间皮瘤的五年生存率低于10%,是一种侵袭性癌症,对许多临床治疗方法均表现出抵抗力。我们首次证明,与化疗相比,双重免疫疗法显示出优越的持续总体生存获益”。
Bristol Myers Squibb的Sabine Maier博士表示:“在超过15年的时间里,对于恶性胸膜间皮瘤患者,尚未批准能够延长生存期的新疗法。我们期待着未来几个月与全球卫生当局就CheckMate -743的积极成果进行讨论”。
原始出处:
http://www.pharmatimes.com/news/opdivoyervoy_improves_survival_in_pleural_mesothelioma_1346650
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#存活率#
35
#胸膜#
41
#Opdivo#
45
#Yervoy#
46
#间皮瘤#
35