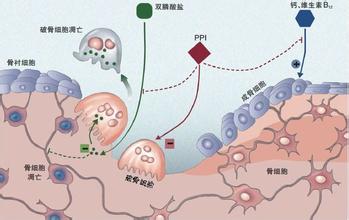
JACC:质子泵抑制剂可用于需要联合抗血小板治疗的胃肠道保护
2016-05-31 phylis 译 MedSci原创
背景:COGENT(氯吡格雷和胃肠道事件的优化试验)表明,在双联抗血小板治疗(DAPT)中,质子泵抑制剂(PPI)可安全减少胃肠道(GI)事件的发生。然而,适当的预防性使用PPI治疗仍然不是最理想,尤其是低剂量的阿司匹林。目标:研究者调查在接受DAPT的低和高剂量阿司匹林亚群,应用PPI治疗的安全性和有效性。方法:在COGENT试验(n = 3752)中,患者随机接受阿司匹林的剂量信息,“低剂量”
背景:COGENT(氯吡格雷和胃肠道事件的优化试验)表明,在双联抗血小板治疗(DAPT)中,质子泵抑制剂(PPI)可安全减少胃肠道(GI)事件的发生。然而,适当的预防性使用PPI治疗仍然不是最理想,尤其是低剂量的阿司匹林。
目标:研究者调查在接受DAPT的低和高剂量阿司匹林亚群,应用PPI治疗的安全性和有效性。
方法:在COGENT试验(n = 3752)中,患者随机接受阿司匹林的剂量信息,“低剂量”(≤100mg)和“大剂量”(>100mg)阿司匹林组。原发性胃肠道终点为上消化道事件,心血管终点是主要不良心脏事件。所有事件都是独立的,对消化科医生和心脏病医生实行盲法。
结果:随访时间的中位数为110天。低剂量阿司匹林的应用者(66.1% ;2480例)老年人、女性、外周动脉疾病史、中风史、高血压较多;而高剂量阿司匹林的使用者(33.9%;1272)高脂血症、吸烟、经皮冠状动脉介入治疗史较多,并超过两倍,美国入组的患者超过两倍(80.4% vs 39.8%)。高剂量的阿司匹林和低剂量组的阿司匹林,180天卡普兰迈耶估计判定复合GI事件(1.7% vs. 2.1%;aHR:0.88;95%CI:0.46至1.66)和主要心脏不良事件(4.8% VS 5.5%;aHR:0.73;95%CI:0.48~1.11)的发生一致。随机化进行PPI治疗可降低低剂量和高剂量阿司匹林组患者,180天Kaplan-Meier估计的主要GI终点(1.2% vs. 3.1%)的发生,对主要心血管终点没有产生不利影响(0.9% vs 2.6%)。
结论:PPI保护胃肠道的治疗适用于冠心病需要DAPT治疗的患者,即使患者应用低剂量的阿司匹林。
原始出处:
Vaduganathan M, Bhatt DL, et al. Proton-Pump Inhibitors Reduce Gastrointestinal Events Regardless of Aspirin Dose in Patients Requiring Dual Antiplatelet Therapy. J Am Coll Cardiol. 2016 Apr 12
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#质子泵#
42
#抑制剂#
41
#JACC#
33
#ACC#
33
#胃肠道#
48
#联合抗血小板治疗#
39