Neurology:血浆可溶性二肽基肽酶4与缺血性卒中后主要心血管事件的风险:中国急性缺血性卒中抗高血压试验(CATIS)的二次分析
2022-07-30 Naomi MedSci原创
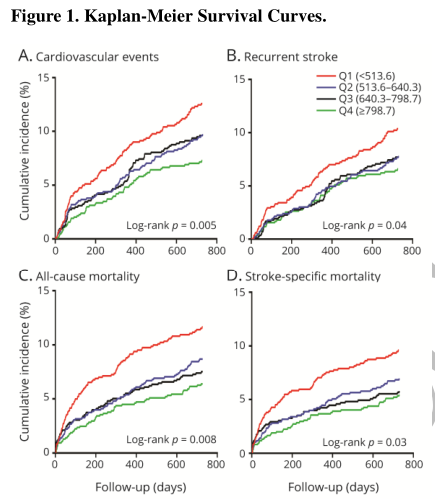
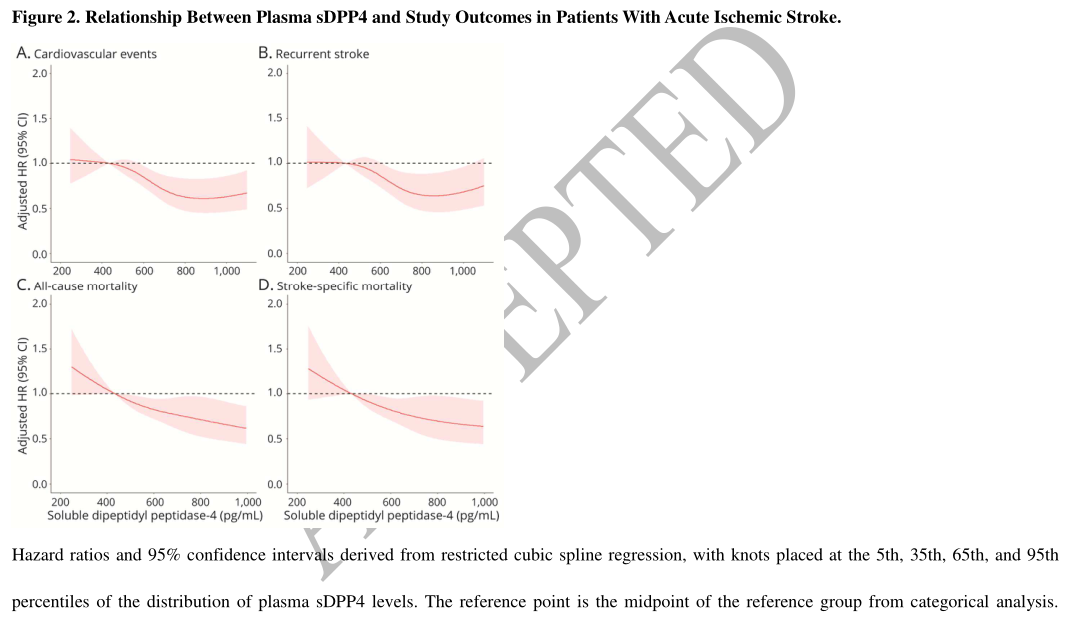
研究发现急性缺血性卒中患者血浆sDPP4水平较高与缺血性卒中后心血管事件、复发性卒中、全因死亡率和功能不良结局的风险降低相关,这表明血浆sDPP4可能是急性缺血性卒中患者初始危险分层的潜在预后标志物。
最近的研究表明,血浆可溶性二肽基肽酶-4 (sDPP4)具有重要的生理效应,可能影响缺血性卒中的预后。近日,一项发表在Neurology上的研究旨在检测急性缺血性卒中患者血浆sDDP4水平与长期临床结果之间的关系。
对来自中国急性缺血性卒中降压试验的3564名参与者(2270名男性和1294名女性)进行了二次分析血浆sDPP4水平的基线测量。使用逻辑回归和Cox回归模型评估了血浆sDPP4水平和2年临床结果之间的关系。通过计算净重新分类指数(NRI)和综合辨别改善(IDI)进一步研究了sDPP4的预测效用。
- 最高的血浆sDPP4四分位数与心血管事件(HR 0.62,95% CI 0.45-0.87)、复发性卒中(HR 0.70,95% CI 0.49-0.99)、全因死亡率(HR 0.62,95% CI 0.44-0.87)、卒中特异性死亡率(HR 0.65,95% CI 0.44-0.94)和不良功能结局(OR 0.66,95% CI 0.97)的风险较低相关。
- 在传统的危险因素模型中加入血浆sDPP4显著改善了所有结果的风险预测。
这项研究发现急性缺血性卒中患者血浆sDPP4水平较高与缺血性卒中后心血管事件、复发性卒中、全因死亡率和功能不良结局的风险降低相关。这些发现表明血浆sDPP4可能是急性缺血性卒中患者初始危险分层的潜在预后标志物。
文献来源:
You S, Miao M, Lu Z, et al. Plasma-Soluble Dipeptidyl Peptidase 4 and Risk of Major Cardiovascular Events After Ischemic Stroke: Secondary Analysis of China Antihypertensive Trial in Acute Ischemic Stroke (CATIS) [published online ahead of print, 2022 Jun 2]. Neurology. 2022;10.1212/WNL.0000000000200784. doi:10.1212/WNL.0000000000200784
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#缺血性卒#
43
#血管事件#
41
#抗高血压#
38
#Neurol#
26
#卒中后#
40
#缺血性#
30
#主要心血管事件#
30