JCO:立体定向放疗或将是非手术治疗肝细胞癌的**!
2015-12-03 zhaozhou 译 MedSci原创
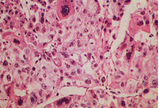
目前对于肝细胞癌(Hepatocellular carcinoma, HCC)的标准治疗方案是进行手术治疗,但是大多数HCC患者并不是适合接受手术治疗,而是接受非手术局部干预治疗。这些治疗方法包括了区域性动脉治疗和局部消融治疗,包括射频消融治疗(RFA)、立体定向放射治疗(SBRT)、经皮乙醇注射(PEI)、微波消融以及冷冻消融。 来自密歇根大学的研究人员对比了SBRT和RF
目前对于肝细胞癌(Hepatocellular carcinoma, HCC)的标准治疗方案是进行手术治疗,但是大多数HCC患者并不是适合接受手术治疗,而是接受非手术局部干预治疗。这些治疗方法包括了区域性动脉治疗和局部消融治疗,包括射频消融治疗(RFA)、立体定向放射治疗(SBRT)、经皮乙醇注射(PEI)、微波消融以及冷冻消融。
原始出处:
Daniel R. Wahl et al. Outcomes After Stereotactic Body Radiotherapy or Radiofrequency Ablation for Hepatocellular Carcinoma. Journal of Clinical Oncology. Published Ahead of Print on November 30, 2015 as 10.1200/JCO.2015.61.4925
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#细胞癌#
23
#JCO#
36
#肝细胞#
30
#立体定向#
33
有意思
116
赞一个
102
好文章,值得收藏
104
#定向#
36
尽管这些数据是前瞻性的,但是SBRT很有可能成为非手术治疗HCC的一线疗法
146
#手术治疗#
26