Neurology:朱永坚团队发现自发性脊柱硬膜外血肿的预后因素
2022-08-27 MedSci原创 MedSci原创
SSEH的不良预后因素可能包括胸段位置、使用抗凝血剂、入院时严重的神经功能障碍、括约肌功能障碍和快速进展。
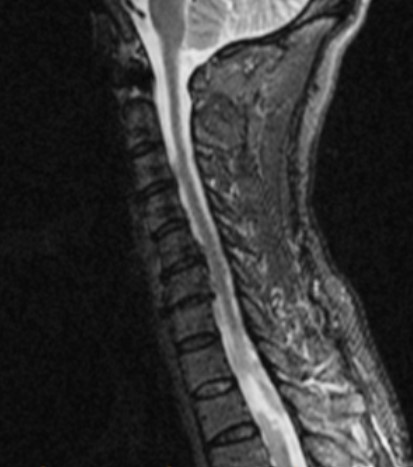
自发性脊柱硬膜外血肿(SSEH)是一种不常见但严重的疾病,发病率高。尽管SSEH与许多风险因素有关,但其病因仍不清楚。关于其预后因素的数据也很匮乏。在本研究中旨在评估SSEH的预后因素。
研究人员对2010年1月至2021年6月在3个学术性神经外科中心因SSEH入院的患者进行回顾性研究。收集了临床参数,包括入院时的临床状况、抗凝血剂的使用、成像方式、进行手术的时间和类型,以及结果。对预后因素进行了分析。用Frankel量表来评估临床状况。
从医疗记录中共检索到105名SSEH患者,平均年龄为51.3岁。83名患者(79%)诉说有急性发作的严重颈部或背部疼痛。82名患者(78%)患有中度至重度神经功能障碍(Frankel量表A-C)。20%的病例发现有抗凝血剂的使用。发现胸椎较低(p = 0.046)、使用抗凝血剂(p = 0.019)、括约肌功能障碍(p = 0.008)、入院时严重的神经功能障碍(p < 0.001)和快速恶化(<1小时,p = 0.004)与不良结果有关。

74个(70%)病例进行了手术减压。单变量和多变量分析显示,术前严重的神经功能障碍(p = 0.005)和截瘫时间延长(>12小时,p = 0.004)是独立的不良预后因素。单变量分析显示,胸椎位置较低(p = 0.08)和快速进展(<6小时,p = 0.005)与预后不良相关,但多变量分析未能确定它们是独立的预后因素。
SSEH的不良预后因素可能包括胸段位置、使用抗凝血剂、入院时严重的神经功能障碍、括约肌功能障碍和快速进展。
参考文献:
Prognostic Factors and Treatments Efficacy in Spontaneous Spinal Epidural Hematoma A Multicenter Retrospective Study.DOI: https://doi.org/10.1212/WNL.0000000000200844
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#硬膜外#
50
#Neurol#
42
#硬膜外血肿#
46
#血肿#
41
#预后因素#
35
#自发性#
32