EUR J Cancer:外周血CD8效应记忆T细胞与ipilimumab治疗的IV期黑素瘤结果具有相关性
2017-12-31 MedSci MedSci原创
记忆T细胞(TM),是人体免疫细胞。人体免疫的第三道防线中分为两部分,一是体液免疫、二是细胞免疫。T细胞分裂和分化后,会分别形成记忆T细胞和效应T细胞,而记忆T细胞则会在下一次抗原入侵时再次将记忆中的杀毒方法再次调动出来,再次破坏靶细胞即受病菌或病毒感染的一般,释放出靶细胞中的抗原。
记忆T细胞(TM),是人体免疫细胞。人体免疫的第三道防线中分为两部分,一是体液免疫、二是细胞免疫。T细胞分裂和分化后,会分别形成记忆T细胞和效应T细胞,而记忆T细胞则会在下一次抗原入侵时再次将记忆中的杀毒方法再次调动出来,再次破坏靶细胞即受病菌或病毒感染的一般,释放出靶细胞中的抗原。
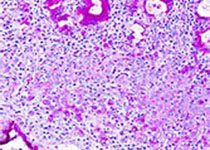
目前尚不清楚外周血中T细胞表型对ipilimumab治疗后的总生存(OS)的影响。为此,研究人员分析了137例晚期黑素瘤患者血液中单核细胞在ipilimumab治疗不同时间点的情况。结果显示, I型CD8效应记忆(EM1)T细胞的高频出现(>13%)标志这更长的OS(p <0.029)和更高的临床缓解率(p <0.01)。这些EM1细胞的出现频率和M型分类对OS有独立的影响(HR=1.5,p=0.033;HR=1.9,p=0.007)。相反,晚期分化效应记忆CD8细胞的高频出现(> 23.8%)与OS呈负相关(p=0.034),但与临床响应无关。
该项试验的观察结果显示,CD8 EM1细胞和CD8细胞的变化是ipilimumab治疗效果的重要的临床表征。
原始出处:
Wistuba-Hamprecht,
Kilian, et al. "Peripheral CD8 effector-memory type 1 T-cells correlate
with outcome in ipilimumab-treated stage IV melanoma patients." European
Journal of Cancer 2017 73: 61-70. doi.org/10.1016/j.ejca.
本文系梅斯医学(MedSci)原创编译整理,转载需授权
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#相关性#
27
#mAb#
32
#Ipilimumab#
22
#黑素瘤#
26
#外周血#
40
#CD8#
21