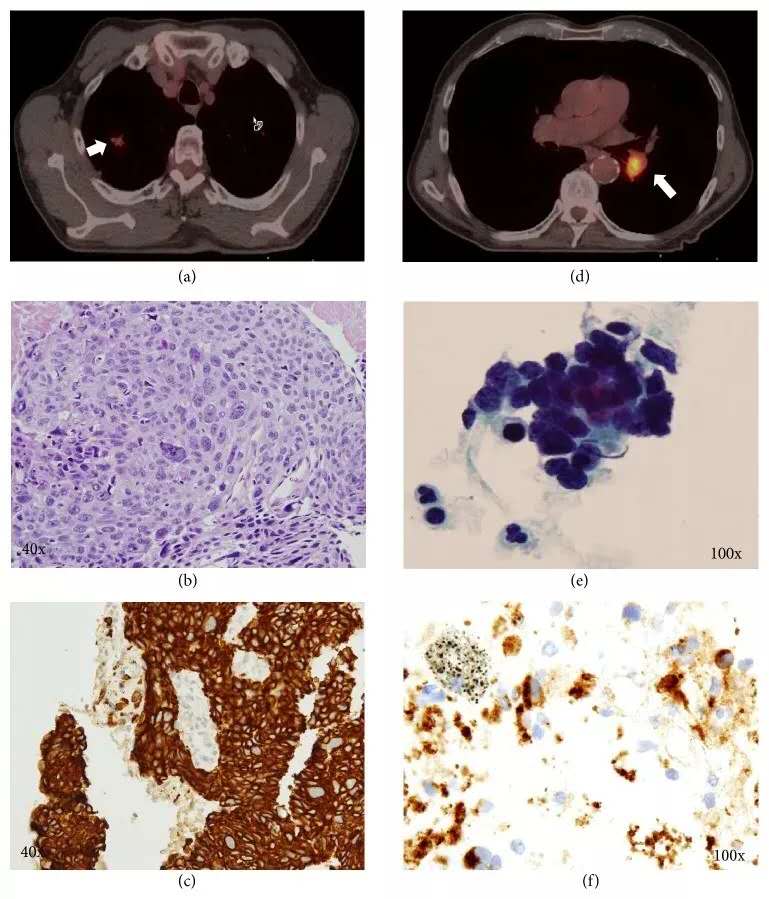
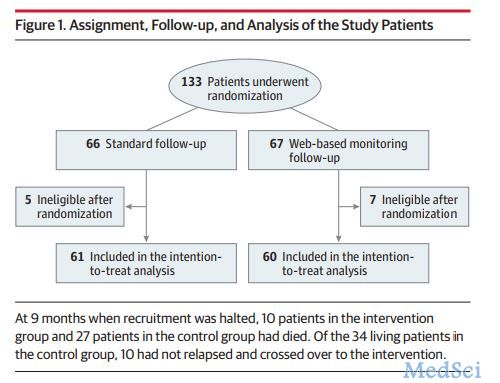
本研究报道了希望之城癌症中心(加利福尼亚州杜阿尔特)和CIRECA,LLC(马萨诸塞州剑桥市)之间合作肺癌研究的结果,该研究包括来自249名患者的328个样本,使用光谱组织病理学的光学技术(SHP)对这些样本进行组织分类。由于SHP基于物理测量,因此与基于评估细胞形态和组织结构的方法相比,它可在更客观和可重复的基础上进行诊断。
该报告表明,SHP提供了可区别与肺鳞状细胞癌的腺癌,其准确性与免疫组织化学和腺鳞癌的高度可靠分类差不多。此外,该报告显示SHP可用于解决肺病理学中观察者之间的差异。光谱组织病理学是基于检测生化组成的变化而不是形态学特征,因此更类似于诸如基质辅助激光解吸电离飞行时间质谱成像的方法。基质辅助激光解吸电离飞行时间质谱和SHP成像模式都表明,在经典病理学中观察到的组织形态学特征的变化伴随着细胞水平的生化组成变化,并且可能与其相关。因此,这些成像方法提供了对疾病引起的生化变化的新见解。
原始出处:
Ali Akalin, Ayşegül Ergin, Resolving
Interobserver Discrepancies in Lung Cancer Diagnoses by Spectral Histopathology
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#组织病理学#
40
#Pathol#
27
学习了
79
#病理学#
34
#Med#
0