Ann Intensive Care:高强度与低强度NPPV对AECOPD患者的生理影响
2022-05-31 小文子 MedSci原创
高强度NPPV在降低AECOPD患者的PaCO2、吸气费力,缓解呼吸困难,改善意识和NPPV耐受性方面是否比低强度NPPV更有效?
无创正压通气(NPPV)越来越多地应用于慢性阻塞性肺疾病急性加重期(AECOPD)患者的治疗。高强度NPPV是一种限制通气的形式,IPAP水平通常在20~30 cmH2O之间,作为一种新的通气方式被引入,通过逐步提高IPAP,最大限度降低升高的PaCO2至正常水平。然而,没有数据表明AECOPD患者应用高强度NPPV是否优于低强度NPPV。Annals of Intensive Care杂志发表的一项研究探索了高强度NPPV在降低AECOPD患者的PaCO2、吸气费力,缓解呼吸困难,改善意识和NPPV耐受性方面是否比低强度NPPV更有效。

研究人员将24例AECOPD患者随机分为高强度NPPV(n = 12)和低强度NPPV(n = 12)两组。在高强度NPPV组,最初以1~2 cmH2O的增量/减量调整IPAP,通常范围为20~30 cmH2O(或可耐受的最大值),以获得10~15mL/kg预测体重的潮气量和 < 25次/min的呼吸速率。在低强度NPPV组以及6小时筛选期间,根据患者的耐受性,IPAP最初以1~2 cmH2O(最高可达20 cmH2O)的增量/增量进行调整,以获得6~10mL/kg预测体重的潮气量和 < 25次/min的呼吸速率。
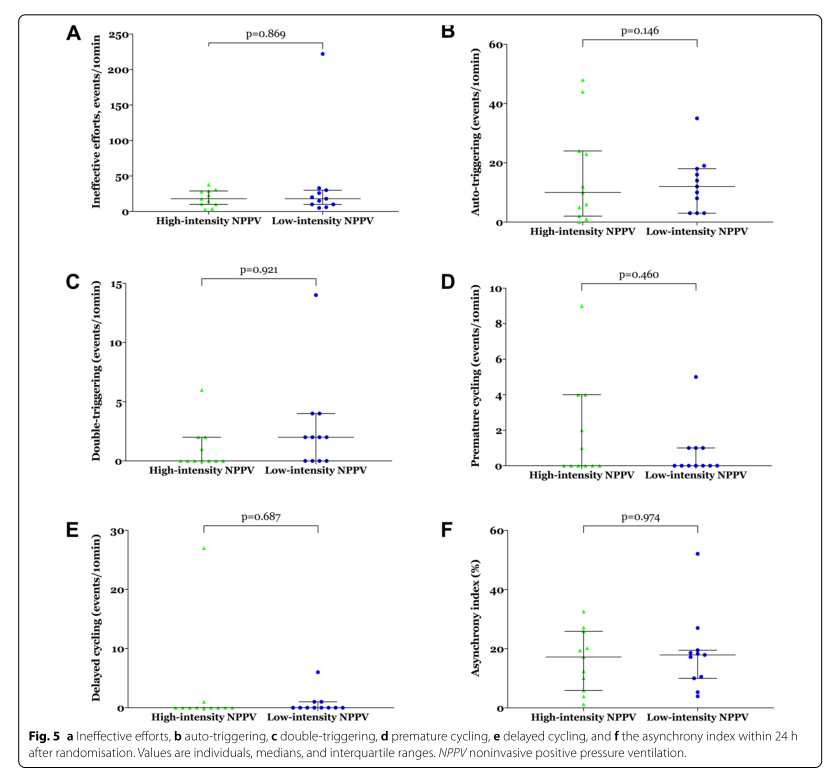
主要结局是随机分组后24小时的PaCO2。次要结局为气体交换、吸气费力、呼吸困难、意识、NPPV耐受性、人机不同步、心功能、呼吸机诱导的肺损伤和NPPV相关不良事件。
结果显示,随机分组24h后,高强度NPPV组的吸入气道正压显著升高(28.0 [26.0~28.0] vs 15.5 [15.0~17.5] cmH2O;p=0.001);随机分组24h内,高强度NPPV组的NPPV持续时间显著长于低强度NPPV组(21.8±2.1 vs 15.3±4.7h;p = 0.001)。随机分组24小时后,高强度NPPV组PaCO2降至54.0±11.6mmHg,而低强度NPPV组仅降至67.4±10.6 mmHg(p = 0.008)。高强度组呼吸-食管压力波动、食管压力-时间乘积(PTPes)/呼吸、PTPes/min、PTPes/L明显降低。随机分组后24h的副肌使用和呼吸困难评分也显著降低。两组间意识、NPPV耐受性、人机不同步、心功能、呼吸机诱导的肺损伤、NPPV相关不良事件均无差异。
结果表面,在降低AECOPD患者PaCO2升高、减少吸气费力和缓解呼吸困难方面,高强度NPPV比低强度NPPV更有效。
原文出处:
Zujin Luo, Zhixin Cao,et al, Physiological effects of high-intensity versus low-intensity noninvasive positive pressure ventilation in patients with acute exacerbation of chronic obstructive pulmonary disease: a randomised controlled trial. Annals of Intensive Care, 2022, https://doi.org/10.1186/s13613-022-01018-4.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







.jpg)





#TENS#
49
#COPD患者#
38
#AECOPD#
38
#高强度#
49
认真学习了
62