新型PARP抑制剂Stenoparib:在临床前研究中显示出抗新冠病毒活性!
2020-08-26 Allan MedSci原创
一系列的临床前研究表明,Stenoparib在LLC-MK2细胞中显示对冠状病毒SARS-Cov-2的抑制活性。
制药公司Oncology Venture今日宣布,其新型PARP抑制剂Stenoparib(以前称为2X-121)已在北亚利桑那大学(NAU)的病原体和微生物组研究所进行了临床前研究,结果显示,Stenoparib具有抗冠状病毒的体外活性。基于这些发现,Oncology Venture计划将该化合物作为COVID-19的潜在疗法推进到人体临床试验。
Stenoparib(2X-121)是Poly ADP-核糖聚合酶(PARP)的新型小分子(口服)靶向抑制剂,PARP是一种在癌细胞中活跃的关键DNA损伤修复酶,PARP-1的缺失使细胞对DNA损伤因子易感, 可能参与肿瘤的发生。
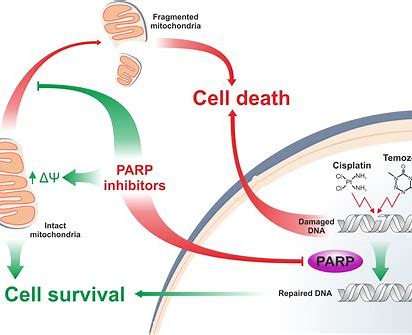
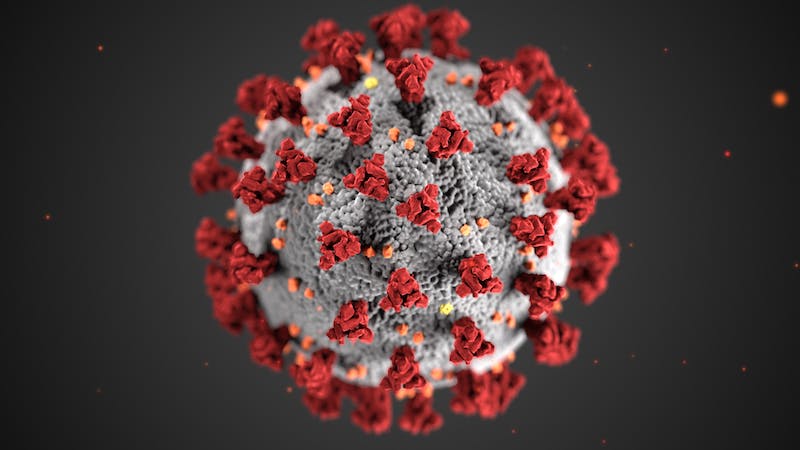
一系列的临床前研究表明,Stenoparib在LLC-MK2细胞中显示对冠状病毒SARS-Cov-2的抑制活性。此外,Stenoparib与remdesivir联用可有效抑制VERO E6细胞中的SARS-Cov-2病毒,两种药物通过独特但不同的作用机制靶向病毒:Remdesivir会阻断RNA复制酶,而Stenoparib作为PARP1 / PARP2(聚ADP-核糖聚合酶)和tankyrase 1和2的抑制剂会抑制病毒的装配,并抑制病毒感染对人体的负面影响,例如细胞因子风暴。
Oncology Venture首席执行官Steve R. Carchedi说:“我们对Stenoparib的临床前研究结果感到非常兴奋,这项研究表明它有望称为COVID-19的潜在疗法。我们打算与FDA和NIH合作,尽快将Stenoparib推进到COVID-19临床试验”。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#病毒活性#
53
学习了
0
#抑制剂#
16
#PARP#
20
标记一下回头来看
133
PARP抑制剂很有前景
138
学习了
121
相关资讯请继续分享,谢谢
94
很好很详细,谢谢分享
63
学习了
43