Int J Mol Med:研究揭示缺乏内源性甲状旁腺激素影响骨折愈合的机制
2018-04-11 MedSci MedSci原创
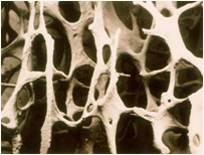
据报道,间歇性低剂量甲状旁腺激素(PTH)注射可以发挥骨合成代谢作用并促进骨折愈合。作为一种重要的促血管生成细胞因子,血管内皮生长因子(VEGF)由骨髓间充质干细胞(BMSCs)和成骨细胞分泌,并在血管发育和再生过程中起重要调节作用。为了研究缺乏内源性PTH是否会导致血管生成能力降低并且由此通过下调VEGF信号传导途径来延迟骨折愈合的过程,研究使用PTH敲除(PTHKO)的小鼠骨折模型。使用X射线
据报道,间歇性低剂量甲状旁腺激素(PTH)注射可以发挥骨合成代谢作用并促进骨折愈合。作为一种重要的促血管生成细胞因子,血管内皮生长因子(VEGF)由骨髓间充质干细胞(BMSCs)和成骨细胞分泌,并在血管发育和再生过程中起重要调节作用。
为了研究缺乏内源性PTH是否会导致血管生成能力降低并且由此通过下调VEGF信号传导途径来延迟骨折愈合的过程,研究使用PTH敲除(PTHKO)的小鼠骨折模型。使用X射线和微型计算机断层摄影术观察骨折愈合。通过免疫组织化学和蛋白质印迹分析来分析骨合成代谢和血管生成标志物。通过定量聚合酶链式反应和蛋白质印迹分析测量小鼠BMSCs衍生的成骨细胞中VEGF的表达水平和相关的信号传导途径。
结果显示,蛋白激酶A(PKA)、磷酸化丝氨酸/苏氨酸蛋白激酶(pAKT)、缺氧诱导因子-1α(HIF1α)和VEGF的表达水平在来自PTHKO小鼠的BMSC衍生的成骨细胞中明显降低。另外,通过免疫组织化学测定,PTHKO小鼠中血小板内皮细胞粘附分子阳性染色减少。PTHKO小鼠中HIF1α、VEGF、Runt相关转录因子2、骨钙素和碱性磷酸酶的表达水平也下降,骨折愈合延迟。
总之,缺乏内源性PTH可能通过下调PKA/pAKT/HIF1α/EGF通路的活性来降低BMSC衍生的成骨细胞中VEGF的表达,从而通过导致血管生成和骨生成的减少而影响软骨内骨形成,最终导致延迟骨折愈合。
原始出处:
Ding Q, Sun P, et al., Lack of endogenous parathyroid hormone delays fracture healing by inhibiting vascular endothelial growth factor‑mediated angiogenesis. Int J Mol Med. 2018 Apr 3. doi: 10.3892/ijmm.2018.3614.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#骨折愈合#
42
#内源性#
25
#甲状旁腺#
33
#Med#
38