Nucleic Acids Res:宿主限制因子与肠道病毒EV71相互作用方面新进展
2018-09-28 ipsvirus 病毒学界
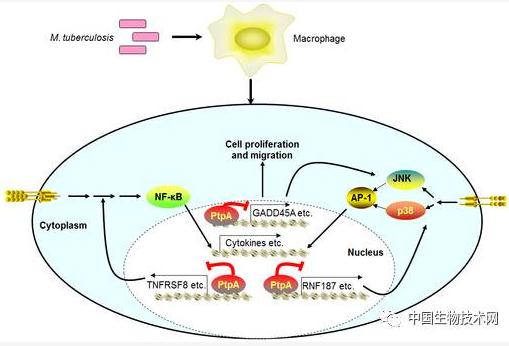
该研究揭示了APOBEC3G(A3G)通过与病毒复制必需的PCBP1竞争结合EV71的5‘UTR序列,抑制EV71在宿主细胞中的复制及翻译,首次揭示了A3G对小RNA病毒的抑制作用,为A3G广谱抗病毒增加新成员。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#EV71#
30
#相互作用#
34
#acid#
38
#CID#
0
#宿主#
35
#肠道病毒#
45
#互作#
22