BMC Cancer:曲妥珠单抗和氟维司群联合治疗HR+/HER2+转移性乳腺癌患者的疗效和安全性
2022-01-14 yd2015 MedSci原创
研究表明,曲妥珠单抗和氟维司群联合治疗HR+/HER2+转移性乳腺癌患者的安全有效,可作为该人群标准抗HER2治疗进展后的一种选择。
曲妥珠单抗和氟维司群联合治疗是激素受体(HR)和人表皮生长因子受体2 (HER2)阳性转移性乳腺癌患者的治疗选择之一;然而,目前评估这种联合疗法疗效的研究还很有限。因此,有国外开展回顾性研究,评估曲妥珠单抗和氟维司群联合治疗HR+/HER2+转移性乳腺癌患者的疗效和安全性。相关结果发表在BMC Cancer杂志上。
研究回顾性收集了1997年8月-2020年8月期间接受曲妥珠单抗和氟维司群联合治疗的HR+/HER2+转移性乳腺癌患者的数据。本研究的主要终点为无进展生存期,次要终点为缓解率、总生存期和安全性。
研究筛查了1612例复发或转移性乳腺癌患者的资料,其中118例患者诊断为HR+/HER2+乳腺癌。其中,28名接受曲妥珠单抗和氟维司群联合治疗。中位年龄66岁(范围50 ~ 80岁)。28例患者中,7例(25%)为新发IV期,21例(75%)为复发。21例(75%)发生内脏转移,包括肝转移和脑转移。
在所有患者中均未观察到完全缓解(CR)。部分缓解(PR) 1例,病情稳定(SD) 17例,疾病进展10例。总有效率为4%,疾病控制率(DCR = CR + PR + SD)为64%。
中位无进展生存期(PFS)为6.4个月(95% CI, 3.46 8.17),中位OS为35.3个月(95% CI, 20.0 46.7)。

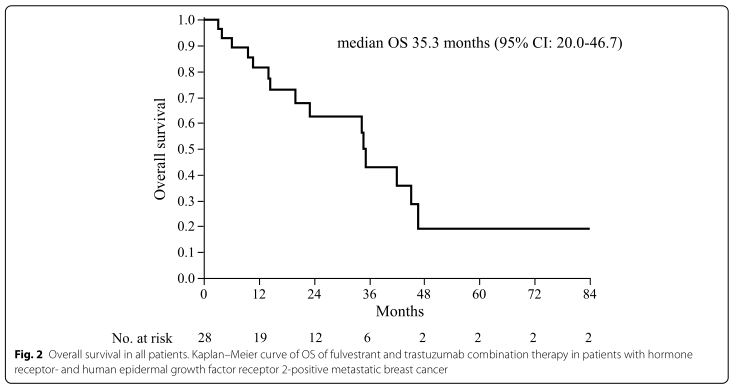
PFS和OS
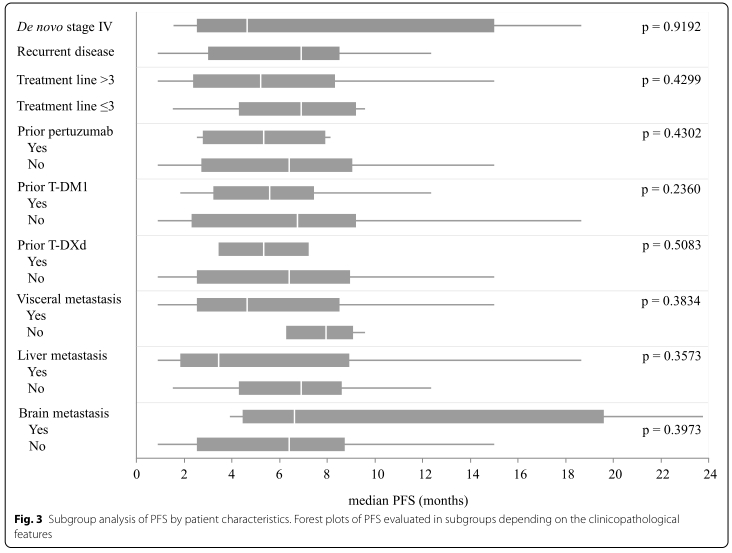
PFS亚组分析
亚组分析,曲妥珠单抗和氟维司群联合治疗作为≤3线治疗患者中,中位无进展生存期(PFS)为7.3个月(95% CI, 1.53-18.67),中位OS未达到。相比之下,作为>3线治疗的患者中位无进展生存期(PFS)为5.2个月(95% CI, 2.57-8.17),中位OS为34.8个月(95% CI, 14.5-45.1)。但是没有显著差异(log-rank检验,p = 0.4299和p = 0.2550)。
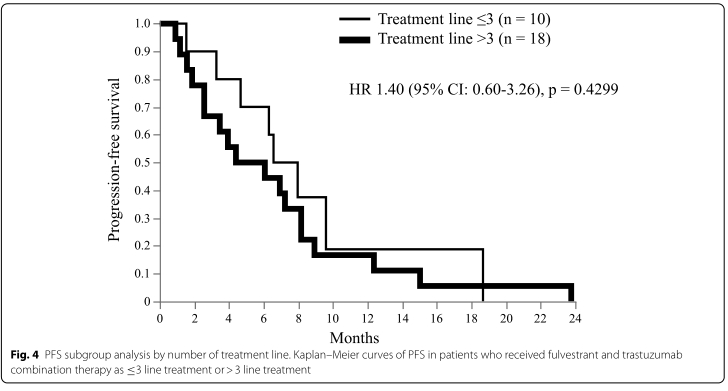
作为不同治疗线数PFS差异
此外,肝转移患者的中位PFS较无肝转移患者的缩短,分别为3.5个月(95% CI, 1.17-8.93)和6.9个月(95% CI, 3.93-8.17) (log rank test, p = 0.3573)。
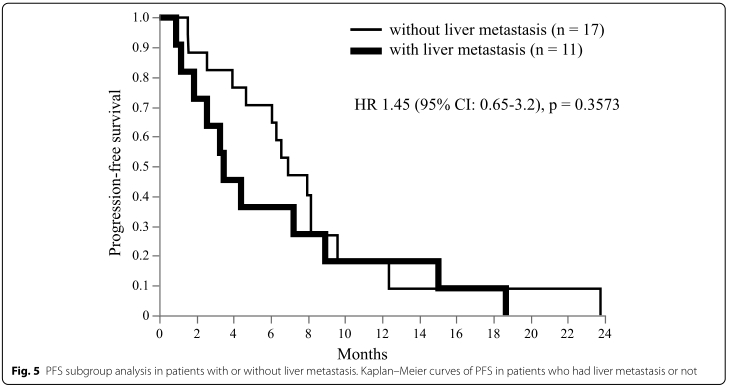
有无肝转移的PFS差异
安全性评估中未观察到3级不良事件。
综上,研究表明,曲妥珠单抗和氟维司群联合治疗HR+/HER2+转移性乳腺癌患者的安全有效,可作为该人群标准抗HER2治疗进展后的一种选择。
原始出处:
Ozaki Y, Aoyama Y, Masuda J, Inagaki L, Kawai S, Shibayama T, Maeda T, Kurata M, Yoshida K, Saeki S, Hosonaga M, Fukada I, Hara F, Kobayashi T, Kobayashi K, Miyake S, Takano T, Ueno T, Ohno S. Trastuzumab and fulvestrant combination therapy for women with advanced breast cancer positive for hormone receptor and human epidermal growth factor receptor 2: a retrospective single-center study. BMC Cancer. 2022 Jan 4;22(1):36. doi: 10.1186/s12885-021-09128-1. PMID: 34983437; PMCID: PMC8728947.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#疗效和安全性#
27
#曲妥珠#
54
#BMC#
25
#联合治疗#
37
#转移性#
27
#乳腺癌患者#
25