Oncologist: HER2阳性胃癌既往曲妥珠单抗治疗进展后继续曲妥珠单抗联合伊立替康治疗并不能增加生存获益
2022-03-23 yd2015 网络
HER2阳性胃癌曲妥珠单抗进展后在伊立替康基础继续联合曲妥珠单抗并未产生明显生存获益,当然,该研究纳入的样本量较少,不足以支持该结论。
近期,Oncologist杂志上发表了一项来自日本的II期临床研究成果,主要是评估HER2阳性胃癌患者曲妥珠单抗联合标准一线化疗治疗进展后,继续曲妥珠单抗联合伊立替康治疗的疗效。
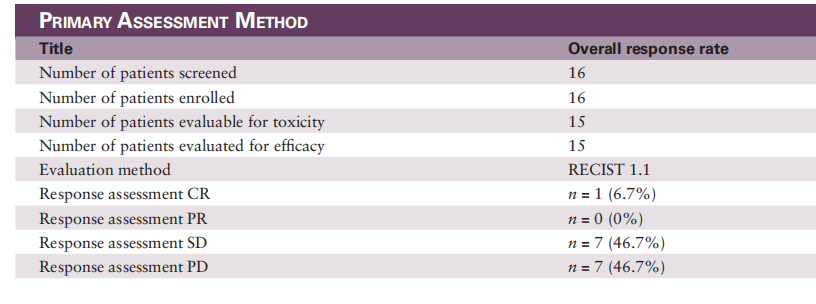
研究纳入的患者每3周接受曲妥珠单抗治疗,以及每2周接受伊立替康治疗。主要终点是总缓解率(ORR),次要终点包括无进展生存期(PFS)、6个月生存率、安全性和HER2状态的亚组分析。
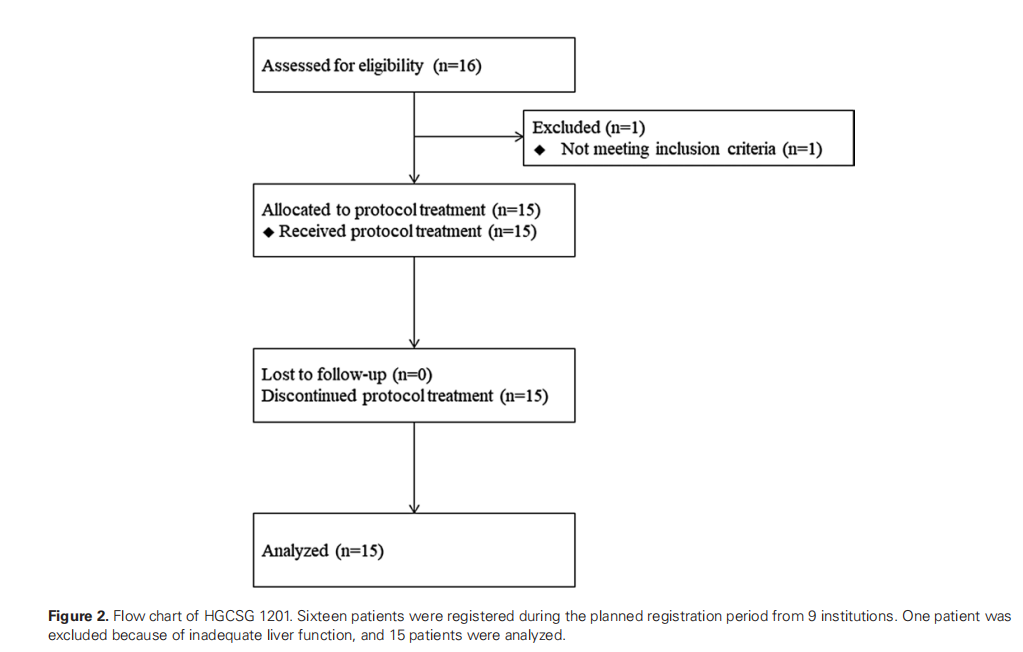
16例患者纳入研究,因纳入患者较少以及疾病控制率不佳而提前结束。ORR和疾病控制率分别为6.7% (95% CI, 0.2 ~ 32.0)和53.3% (95% CI, 26.6 ~ 78.7)。
中位无进展生存期(PFS)和总生存期(OS)分别为2.4个月(95% CI, 0.0-5.2)和9.7个月(95% CI, 8.2-11.2)。其中6个月PFS率为13.3%(95%CI,3.4-40.5)。而6个月和12个月的OS率分别为73.3%(95%CI,46.7-89.6)和26.7%(95%CI,10.4-53.3)。
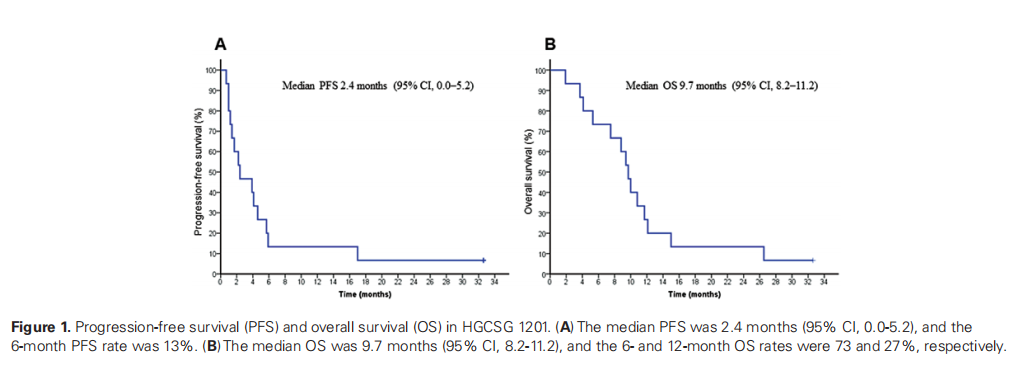
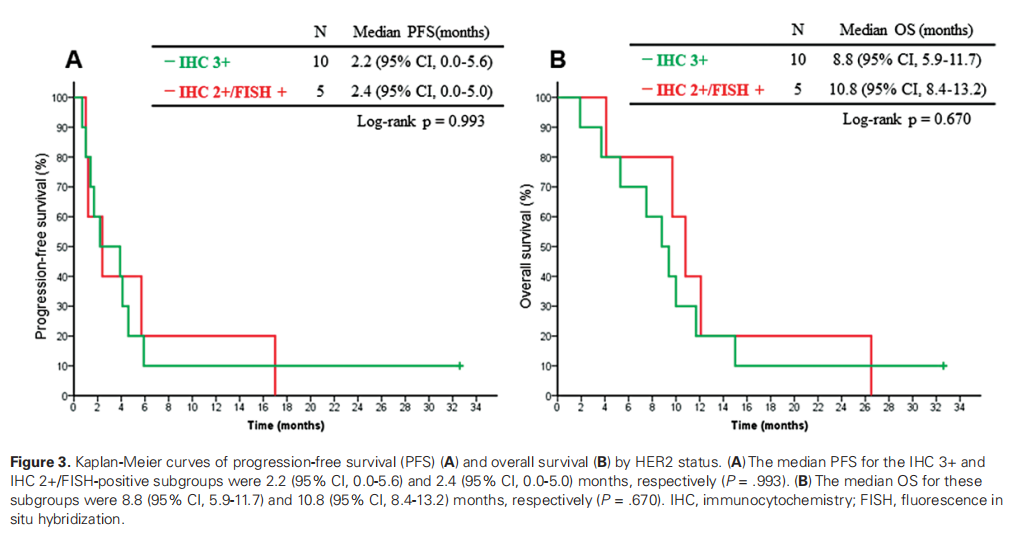
在HER2状态的亚组分析中,IHC3+和IHC2+/FISH阳性亚组的中位PFS分别为2.2个月(95%CI,0.0-5.6)和2.4个月(95%CI,0.0-5.0)(P=0.993)。这些亚组的中位OS分别为8.8个月(95%CI,5.9-11.7)和10.8个月(95%CI,8.4-13.2)(P=0.670)。
最常报道的3-4级不良事件为中性粒细胞减少(40%),贫血(27%),厌食症(33%)和疲劳(33%)。
综上,HER2阳性胃癌曲妥珠单抗进展后在伊立替康基础继续联合曲妥珠单抗并未产生明显生存获益,当然,该研究纳入的样本量较少,不足以支持该结论。
原始出处:
Yasuyuki Kawamoto, Satoshi Yuki, Takashi Meguro, et al. Phase II Study of Continued Trastuzumab Plus Irinotecan in Patients with HER2-positive Gastric Cancer Previously Treated with Trastuzumab (HGCSG 1201). The Oncologist, 2022, XX, 1–8 .https://doi.org/10.1093/oncolo/oyab062.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Oncol#
28
#HER2阳性胃癌#
30
#生存获益#
37
#曲妥珠#
44
#HER2阳性#
57
#GIST#
29