Blood:单细胞DNA扩增测序揭示T-ALL的克隆异质性和进化
2020-08-28 MedSci原创 MedSci原创
急性T淋巴细胞白血病(T-ALL)是一种侵袭性白血病,在儿童中最常见,其特征是在确诊时存在很少的染色体重排,蛋白质编码区域中存在10-20个体细胞突变。大多数T-ALL病例都携带NOTCH1的激活突变
急性T淋巴细胞白血病(T-ALL)是一种侵袭性白血病,在儿童中最常见,其特征是在确诊时存在很少的染色体重排,蛋白质编码区域中存在10-20个体细胞突变。大多数T-ALL病例都携带NOTCH1的激活突变及与激酶信号传导、转录调控或蛋白质翻译有关的基因突变。
为了在诊断和治疗过程中获得更多关于克隆异质性水平的了解,Servera等用Tapestri平台进行了单细胞靶向DNA测序,设计了一个定制的ALL面板,并获得了准确的单核苷酸突变和小片段的插入缺失突变,要求每个样本每次约测4400个细胞、覆盖110个基因。
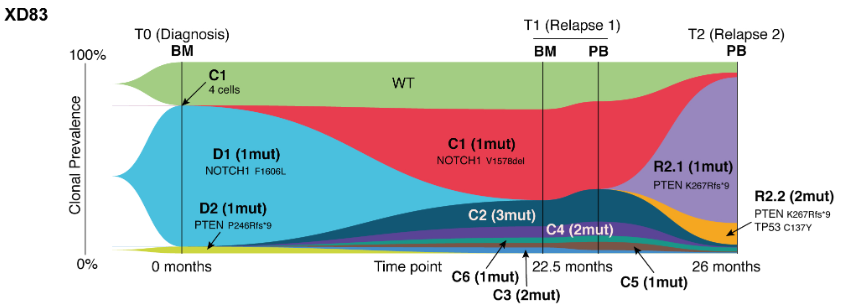
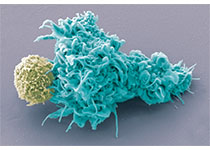
(患者XD83从确诊到复发的克隆变化)
分析了8位T-ALL患者的25个样本共108188个细胞。在诊断时,通常可观察到一个主要克隆(>35%的细胞),并伴有几个次要克隆,其中一些少于细胞总数的1%。四名患者具有>2个NOTCH1突变,其中一些存在于较少的克隆中,表明在发育过程中,T-ALL细胞有较大的获得NOTCH1突变的压力。
通过分析纵向样本,研究人员在确诊时的样本中还检测到了残留白血病细胞以及具有少量存在的克隆的存在及克隆性质,这些克隆在疾病后期逐渐发展为临床相关的主要克隆。
总而言之,单细胞DNA扩增测序是检测T-ALL中克隆结构和进化的灵敏方法。
原始出处:
Llucia Albertí-Servera,et al. Single-cell DNA amplicon sequencing reveals clonal heterogeneity and evolution in T-cell acute lymphoblastic leukemia. Blood. August 18,2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#克隆#
41
学习
87
应用
88
#ALL#
36
#T-ALL#
52