对铜绿假单胞菌有效的抗生素有哪些?这8点请注意!
2022-02-11 刘少飞 呼吸新前沿
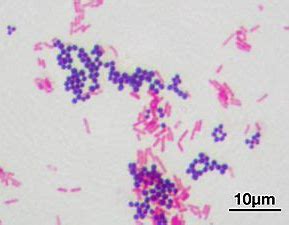
铜绿假单胞菌(pseudomonas aeruginosa)是一种非发酵革兰阴性杆菌,这种病原体可引发严重后果。它在环境中广泛分布,
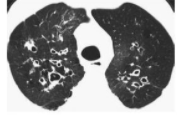
铜绿假单胞菌(pseudomonas aeruginosa)是一种非发酵革兰阴性杆菌,这种病原体可引发严重后果。它在环境中广泛分布,尤其是水中,甚至可以污染蒸馏水;它也是热水浴缸和角膜接触镜护理液污染相关感染的重要病因。铜绿假单胞菌作为一种医院内的潜在病原体已引起了高度重视,因为:
1. 该菌常见于水槽并能污染呼吸设备(可成为环境贮库,尤其是在ICU);
2. 该菌容易感染免疫功能受损的宿主,包括烧伤患者;
3. 该菌是导致呼吸机相关肺炎(ventilator-associated pneumonia, VAP)最严重的病原体;
4. 一些医院和地区已常见耐多药铜绿假单胞菌菌株。

一般原则是使用抗生素,包括抗生素的选择和联合治疗的决策。铜绿假单胞菌感染,首选药物需要根据药敏试验选择。铜绿假单胞菌又称绿脓杆菌,β-内酰胺酶类、氨基糖苷类药物、喹诺酮类药物治疗均可取得相应疗效。然而,铜绿假单胞菌又存在耐药性。
| 铜绿假单胞菌的耐药机制
耐药性的产生是多方面的,该菌能够通过质粒或染色体介导产生包括金属酶、超广谱β-内酰胺酶在内的多种水解酶,导致细菌耐药;该菌能够改变抗菌药物作用靶点并通过能量依赖的主动外排系统将药物排出到细菌体外;另外,该菌还能通过生成生物膜形成天然的耐药屏障。
1.1 产生水解酶;
1.2 改变抗菌药物作用靶点;
1.3 主动外排作用;
1.4 产生生物膜。
| 防治铜绿假单胞菌产生耐药的措施
1 根据药敏试验选用抗生素
对确诊感染铜绿假单胞菌患者,有一定的临床表现及病原学检查依据时,应根据药敏试验选用敏感抗菌药物。
2 评估病原学检查结果
对病原学检查结果要进行评估,确定病原菌是致病菌还是定植菌。机械通气时,气管插管吸出痰液培养出的细菌可以是致病菌,也可以是定植菌。在吞咽功能不良时,上呼吸道的定植菌可以流入下呼吸道。所以对阳性培养结果要结合临床进行评估。考虑为定植菌时原则上不应使用抗铜绿假单胞菌药物。
3 经验性治疗
对未能取得病原学证据但有临床表现及发病条件,怀疑有铜绿假单胞菌感染并决定进行经验性治疗时,可根据本地区本医院近年的铜绿假单胞菌耐药性和敏感性情况选择适当的抗铜绿假单胞菌药物。可分别选择头孢他啶、哌拉西林、哌拉西林/他唑巴坦,或亚胺培南、美罗培南等。应严格控制经验性治疗,但须注意体液免疫功能低下患儿容易发生严重的铜绿假单胞菌感染,应及早选用有力的抗铜绿假单胞菌药物。
4 只对氟喹诺酮类药物敏感的铜绿假单胞菌感染患者的治疗
如患儿发生铜绿假单胞菌感染,对所有β-内酰胺酶类药物耐药,只对氟喹诺酮类药物敏感,此时可考虑使用环丙沙星(由于药品管理条例的一些限制,原则上家属签字后使用为宜)。在使用氟喹诺酮类药物抗铜绿假单胞菌时,选用环丙沙星优于左氧氟沙星。
5 保护性应用抗铜绿假单胞菌药物
目前细菌高度耐药情况产生的重要原因是使用过多广覆盖的抗生素。因此,当不是特别考虑为铜绿假单胞菌感染时应避免使用有抗铜绿假单胞菌作用的抗生素,应保护抗铜绿假单胞菌药物。例如,不应在社区获得性感染中选用头孢他啶。在其他感染中如需使用三代头孢菌素时亦不应选用头孢他啶,以减少耐头孢他啶的铜绿假单胞菌产生。在成人一般感染的治疗中应控制氟喹诺酮类药物的使用。
对尚不考虑铜绿假单胞菌感染和鲍曼不动杆菌感染,而考虑大肠埃希菌和克雷白菌属耐药菌(如产超广谱β-内酰胺酶或头孢菌素酶)导致的感染,并决定使用碳青霉烯类药物时应选择厄他培南,而不是选择亚胺培南或美罗培南,可减少耐药铜绿假单胞菌的产生。
厄他培南的临床价值在于其独特的抗菌谱特点,使其保留了碳青霉烯类药物强大的杀菌活性,可直接用于疑似产超广谱β-内酰胺酶和头孢菌素酶耐药菌引起的感染,同时对非发酵菌无活性,不会造成过度覆盖铜绿假单胞菌,同时不过度覆盖鲍曼不动杆菌,有助于减少由于过度使用抗铜绿假单胞菌药物而产生耐药菌的情况。
6 了解铜绿假单胞菌耐药趋势
医生要了解近期本地区、本医院和本病区耐药菌的情况和变化趋势,对正确运用抗菌药物进行经验治疗有重要意义。
7 合理分配使用抗生素
为控制多药耐药菌株的产生,对医院所在地区、医院一般科室、门诊均应采取抗生素应用的保护策略,以留给ICU和收治重症感染的病区一定的抗生素使用余地。
8 重视消毒、隔离
严格进行医疗器械消毒,医护人员勤洗手,认真执行无菌操作。高度重视医护人员的手卫生,病房各种用具、空气及各种侵入性器械的消毒管理。坚持医院对病原菌耐药性的监测。
参考文献:
1. Ibrahim D, Jabbour JF, Kanj SS. Current choices of antibiotic treatment for Pseudomonas aeruginosa infections. Curr Opin Infect Dis. 2020 Dec;33(6):464-473.
2. Warburton DW, Bowen B, Konkle A. The survival and recovery of Pseudomonas aeruginosa and its effect upon salmonellae in water: methodology to test bottled water in Canada. Can J Microbiol 1994; 40:987.
3. 刘慧慧,李玖军.铜绿假单胞菌耐药机制及耐药性变迁研究进展.中国小儿急救医学, 2014,21(3) : 171-173. DOI: 10.3760/cma.j.issn.1673-4912.2014.03.019
4. 刘又宁, 施毅. 铜绿假单胞菌下呼吸道感染诊治专家共识 [J]. 中华结核和呼吸杂志, 2014.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










耐药铜绿假单单胞菌的治疗,要注意抗生素的保护,一般无耐药菌时,要避免使用头孢他啶,厄他培南,和氟喹诺酮类药物的应用
54
好多铜绿
52
内容不错
57
很有意义,学到了,棒极了
67
学到了
47
有意义
36
很有指导性!
29
内容充实,学习到了
31
学习学习
24