Nat Commun:中国学者提出靶向血管重构治疗肺动脉高压治疗的新策略
2019-09-26 佚名 中国循环杂志
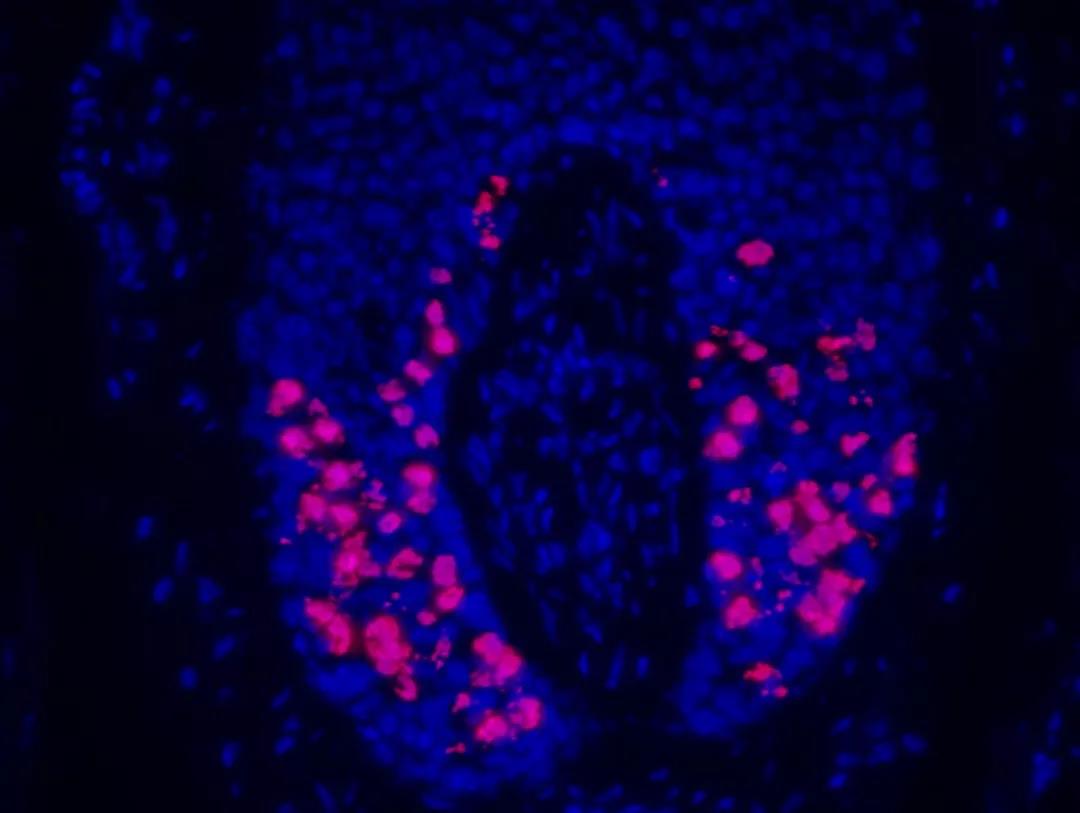
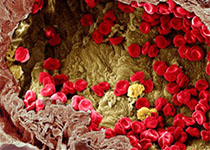
肺动脉高压,是一组心肺血管重塑疾病,预后较差,但尚无法有效逆转肺血管重构。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Nat#
25
#COMMUN#
28
#动脉高压#
32
#血管重构#
35
#高压治疗#
40
谢谢了,学习
59
#新策略#
24
学习学习学习学习
56
肺动脉高压表面是罕见病,事实上临床上并不少见,治疗药物虽然有一些,但是整体仍然不理解,可能未来需要采用综合治疗措施。
41