JACC:肺动脉高压患者,初始治疗选择三联还是二联药物治疗?
2021-10-08 Nebula MedSci原创
肺动脉高压患者,初始治疗选择三联还是二联药物治疗?
肺动脉高压 (PAH) 是一种不断进展的疾病,多种病理生理机制参与促进其发生进展。在已明确的机制中,前列环素、内皮素和一氧化氮途径可以成为药物治疗的靶点。靶向多种途径的联合治疗是 PAH 管理的重要组成部分。
但是,迄今为止,还没有数据对比初始三联口服治疗与二联口服治疗 PAH 的优劣。TRITON 研究是一项多中心、双盲、随机的 3b 期试验,评估了初始三联(马西替坦、他达拉非和司来帕格)对比初始二联(马西替坦、他达拉非和安慰剂)口服疗法在新确诊的未治疗过的 PAH 患者中的疗效。
最后一位随机分组患者完成了 26 周随访后进行疗效评估。主要终点是第 26 周时肺血管阻力 (PVR) 的变化。
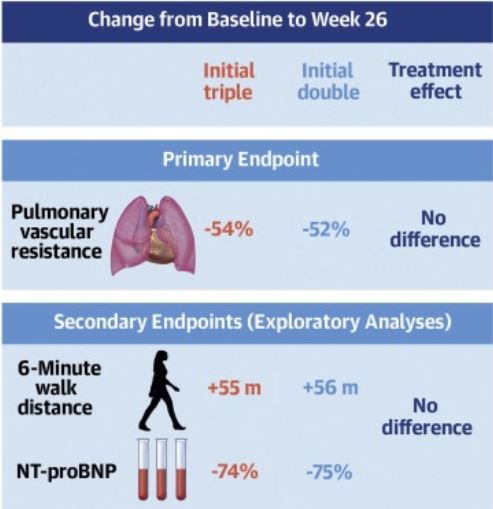
26 周时主要终点和次要终点的结果
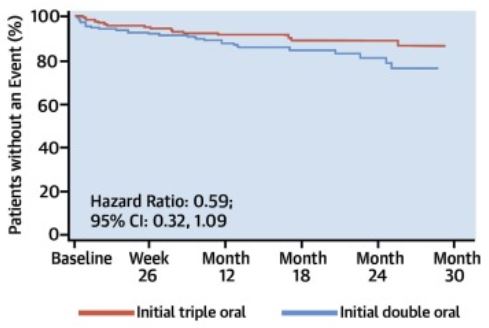
受试患者被随机分至三联组(n=123)或二联组(n=124)。第 26 周时,与基线相比,两种治疗方案都明显降低了受试患者的 PVR(分别降低了 54% 和 52%),两组间无明显差异(几何平均比:0.96;95% CI 0.86-1.07; p=0.42)。第 26 周时,两组的六分钟步行距离和 N-末端 proBNP 均有所改善(组间无明显差异)。与初始二联疗法相比,初始三联疗法显著降低了受试患者的疾病进展风险(风险比 0.59, 95% CI 0.32-1.09)。
两组患者的无事件生存率
初始三联疗法最常见的不良事件包括头痛、腹泻和恶心。截止观察期结束时,初始三联组有两位患者、初始双联组有 9 位患者死亡。
综上所述,两种治疗策略均显著降低了新确诊的 PAH 患者的肺血管阻力(组间无显著差异)。探索性分析显示,初始三联口服治疗相比初始二联口服治疗有望改善 PAH 患者的长期预后。
原始出处:
Chin Kelly M,Sitbon Olivier,Doelberg Martin et al. Three- Versus Two-Drug Therapy for Patients With Newly Diagnosed Pulmonary Arterial Hypertension.[J] .J Am Coll Cardiol, 2021, 78: 1393-1403. https://doi.org/10.1016/j.jacc.2021.07.057
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#治疗选择#
63
#肺动脉高压患者#
53
#初始治疗#
49
#JACC#
38
#动脉高压#
51
#ACC#
32