Blood:HCT后CD4+T细胞重建可预测急性GvHD患者的存活预后
2020-11-18 MedSci原创 MedSci原创
急性移植物抗宿主病(aGvHD)是异基因造血细胞移植(HCT)后引起高死亡率的危及生命的并发症。虽然已应用了多种方案预防aGvHD的发生,但aGvHD仍很常见,约影响20-60%进行异基因HCT的患者
急性移植物抗宿主病(aGvHD)是异基因造血细胞移植(HCT)后引起高死亡率的危及生命的并发症。虽然已应用了多种方案预防aGvHD的发生,但aGvHD仍很常见,约影响20-60%进行异基因HCT的患者。既往研究表明,早期CD4+T细胞重建(CD4+IR)可以预测患者HCT后的存活率。
在该研究中,Coco等研究了CD4+IR与HCT后发生aGvHD的患者的存活率的相关性。纳入了在两个独立的中心(UMC/PMC和MSK)接受首次异基因HCT的儿童患者。主要预后指标是无复发死亡率(NRM)和总存活率(OS),根据aGvHD和CD4+IR分层。应用多变量和事件发生时间Cox比例风险模型。
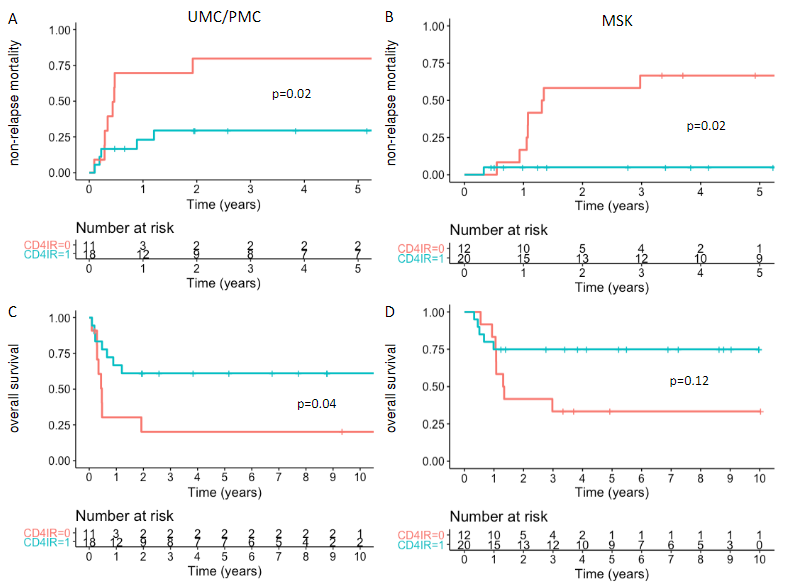
HCT后100天内有无CD4+IR的III-IV级aGvHD患者的无复发死亡率和总体存活率
纳入591例患者(UMC/PMC 276例、MSK 315例)。在HCT后100天内有或无CD4+IR的III-IV级aGvHD患者,UMC/PMC的NRM分别为30% vs 80%(P=0.02),MSK的NRM分别为5% vs 67%(P=0.02)。此外,无CD4+IR还与低OS有关;UMC/PMC组有CD4+IR vs 无CD4+IR的患者的OS为61% vs 20%(p=0.04),MSK组的为75% vs 33%(p=0.12)。aGvHD发病前CD4+IR不足与NRM显著升高(74% vs 12%)、OS较差(24% vs 78%)相关(p均<0.001)。
综上所述,在该回顾分析中,研究人员证明了简单而有力的预测患者HCT后预后的标志物——早期CD4+IR——与中重度aGvHD患者的存活率相关。该研究提示,改善HCT后T细胞恢复的策略可能会影响发生aGvHD患者的存活率。该结果需要进一步通过前瞻性试验进行验证。
原始出处:
de Koning Coco,Prockop Susan,Roessel Ichelle van et al. CD4+ T-cell reconstitution predicts Survival Outcomes after acute Graft-versus-Host-Disease; a dual center validation. Blood, 2020. https://doi.org/10.1182/blood.2020007905
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CD4#
36
#CD4+#
35
#HCT#
38
#CD4+T细胞#
39
学习了
80
学习了
73