JNER:神经系统疾病患者机器人神经康复步行功能预后的预测
2022-01-01 MedSci原创 MedSci原创
神经系统疾病往往是慢性的、使人衰弱的,给家庭和社会带来沉重负担。改善活动能力是神经系统疾病患者康复的主要目标之一 。在神经康复中,高剂量和强度、足够的练习、个性化目标、动机和专业知识都是获得更好结果的
神经系统疾病往往是慢性的、使人衰弱的,给家庭和社会带来沉重负担。改善活动能力是神经系统疾病患者康复的主要目标之一 。在神经康复中,高剂量和强度、足够的练习、个性化目标、动机和专业知识都是获得更好结果的重要因素。与传统疗法相比,机器人辅助步态训练 (RAGT) 有望更有效地改善活动能力,因为它可以提供比常规康复更高的剂量和更密集的治疗。RAGT 与传统步态训练 (CGT) 之间的疗效比较在康复医学中引起了相当大的关注。训练强度、持续时间和训练量以及治疗类型、参与者特征和试验测量的变化可能导致报告的不同有效性水平。然而,使用 RAGT 设备为患者获得最佳效果的具体应用仍不清楚。
定期结果评估和跟踪是实施有效医疗实践的基本方法,并得到中风康复指南的支持。尽管 RAGT 提供了高度密集和重复的特定任务培训,但培训计划也需要个性化和监控以实现有效的神经康复。然而,从正在进行的 RAGT 获得的数据可以最好地组织成预测模型来帮助临床医生、患者及其家人尽早做出决策和规划机器人辅助康复管理。在 Lokomat 训练期间,机械臂提供的体重 (BW) 支撑系统和引导力 (GF) 帮助患者遵循生理步态模式。尚未建立基于 Lokomat 训练数据的预测模型来帮助确定使用该系统的患者恢复步行功能的成本效益方法。这项研究的目的有两个。首先,试图确定在不同恢复阶段的神经系统疾病成年患者中最有益的 RAGT 参数组合。其次,预计会开发预测模型,以评估该人群中基于 Lokomat 疗法的功能性行走类别 (FAC) 的改进。 FAC 是步态相关研究中常用的结果测量方法,是一种六点分类量表,用于评估患者对步态的支持程度。本文发表在《J NeuroEngineering Rehabil》。
回顾性收集了在台北医科大学医院接受 Lokomat 培训的 139 名患者的数据。 在对数据完整性进行筛选后,本研究纳入了 91 名患有急性或慢性神经系统疾病的成年患者的记录。 将来自 Lokomat 的患者特征和定量数据作为特征来构建预测模型,以探索与患者康复相关的早期反应和因素。
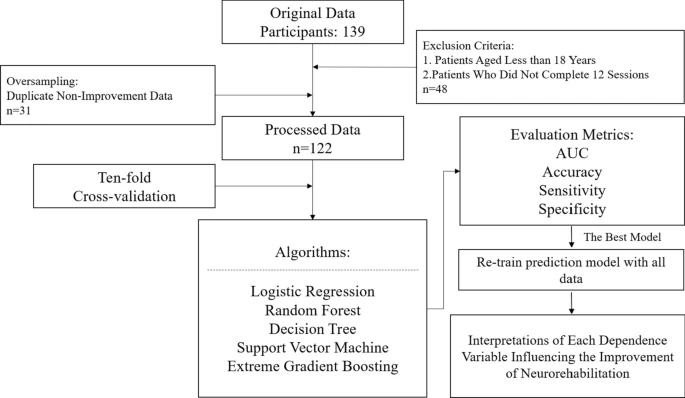
试验流程图
据观察,患者的年龄和完成一节训练的时间(即 12 节 Lokomat 训练,以天为单位)在改善组和未改善组之间没有显着差异。对于 Lokomat 参数,除第一次会话的 GF 外的所有变量都显示出两组之间的显着差异。使用不同数量的训练结果进行十倍交叉验证的不同机器学习算法的预测性能以预测第 12 个会话的 FAC 的结果。所有训练都被选为机器学习算法的输入,以进一步比较预测性能。为了研究分类器之间的 AUC 均值、准确性、敏感性和特异性是否存在显着差异,我采用方差分析 (ANOVA) 来检查差异。来自不同机器学习算法的 AUC 的平均值通过十倍交叉验证对三个水平从高到低排列如下:RF,0.814; XGBoost,0.768;支持向量机,0.724;逻辑回归,0.675;和决策树,0.485。

预测机器人辅助步态训练(RAGT)对功能性步态恢复的有效性
大多数针对急性和亚急性卒中患者的运动康复试验报告说,实验组和对照组的改善程度相同,这表明新发卒中患者可能会在没有特定神经康复方法的情况下自发康复。在这项研究中,提供了一个基于患者特征的动态功能结果的预测模型,这些数据来自基于机器人的治疗的早期定量数据,以减少步行障碍。研究表明,患者的年龄或接受 Lokomat 培训的总天数没有显着的组间差异,这表明基于机器人的神经康复治疗范围更广。 Lokomat 训练通常从 100% 指导开始,以强制执行生理步态模式。这可以解释为什么只有第一次训练的 GF 没有表现出显着的组别差异。对分类变量的描述性统计结果表明,切入点和诊断结果显示出显着差异,这与早期康复改善结果的先前发现一致。
总之,本文根据患者特征和早期机器人神经康复减少损伤的定量数据开发了一个动态结果的预测模型。 RAGT 是一种针对不同情况的患者重新获得行走能力的定制方法。 为了获得更精确、更清晰的预测模型,收集更多的 RAGT 训练参数并针对每种疾病进行分析是一种可能的方法,可以帮助临床医生更好地了解不同患者的最有效 RAGT 参数。
Kuo, CY., Liu, CW., Lai, CH. et al. Prediction of robotic neurorehabilitation functional ambulatory outcome in patients with neurological disorders. J NeuroEngineering Rehabil 18, 174 (2021). https://doi.org/10.1186/s12984-021-00965-6
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#步行#
65
#疾病患者#
49
认真学习了
68
向研究表明,在一次就诊时被确定为MCI的人中,有5%至53%在下一次就诊时不再
70
#神经系统#
48
#机器人#
51
#功能预后#
50
#机器#
51