Primary sclerosing cholangitis,PSC(原发性硬化性胆管炎)
2022-09-14 放射沙龙 英文图书《Liver MRI》
是一种慢性胆汁淤积性肝病,通常与炎症性肠病(IBD)相关(2/3的患者)。特征是肝内和肝外胆管纤维化炎性破坏,最终因肝功能衰竭和胆管癌而导致死亡(10-30%)。
是一种慢性胆汁淤积性肝病,通常与炎症性肠病(IBD)相关(2/3的患者)。
特征是肝内和肝外胆管纤维化炎性破坏,最终因肝功能衰竭和胆管癌而导致死亡(10-30%)。
PSC被认为是多因素和多基因病因的一种免疫介导肝病。可出现肝脏或胆道疾病的症状和体征。从诊断开始,患者就会出现生化胆汁淤积。自身免疫性肝炎和胰腺炎与该病有关。
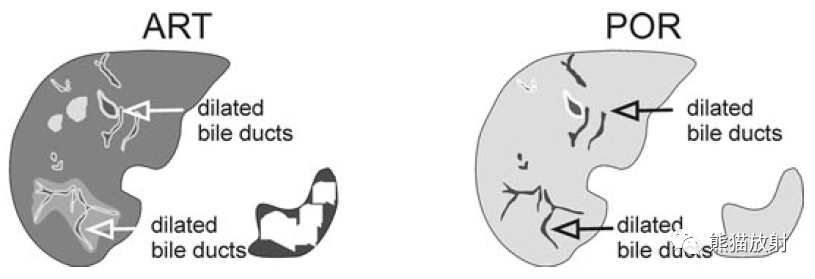
PSC的MRI表现包括:
(1)肝内胆管扩张;
(2)肝内胆管狭窄;
(3)肝内胆管呈串珠状;
(4)T2WI上门静脉周围高信号,动脉期肝脏外围区域的肝实质强化;
(5)肝外胆管壁增厚并强化;
(6)肝外胆管狭窄;
(7)肝节段性肥大,如尾状叶,而其他肝段萎缩;
(8)门静脉周围淋巴结肿大;
(9)胆囊增大。
MRCP和动态增强MR扫描有助于揭示原发性硬化性胆管炎的肝内和肝外特征。
部分肝段的萎缩是由复发性胆管炎和纤维化引起的。

-
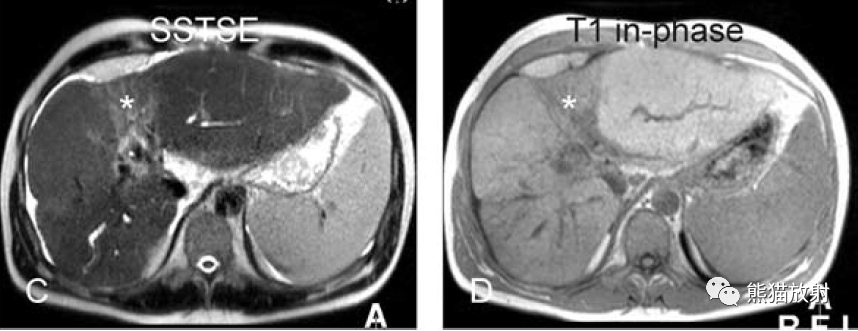
黑血EPI:外周胆管扩张,炎症引起的肝实质性信号增高;正常的肝实质(*);
-
T1同相位:肝实质看似正常;
-
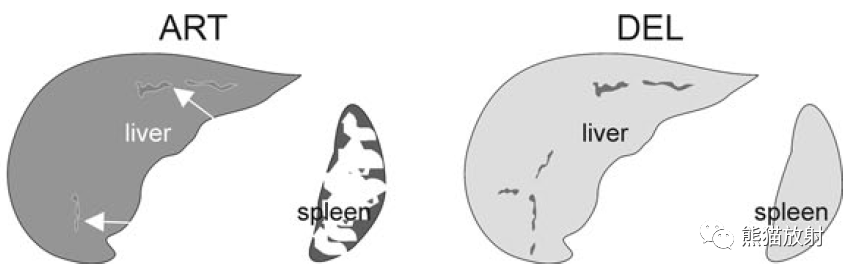
增强动脉期(ART):部分扩张胆管周围肝实质强化明显,提示胆管炎;
-
门脉期(POR):强化区域与正常肝实质一致。
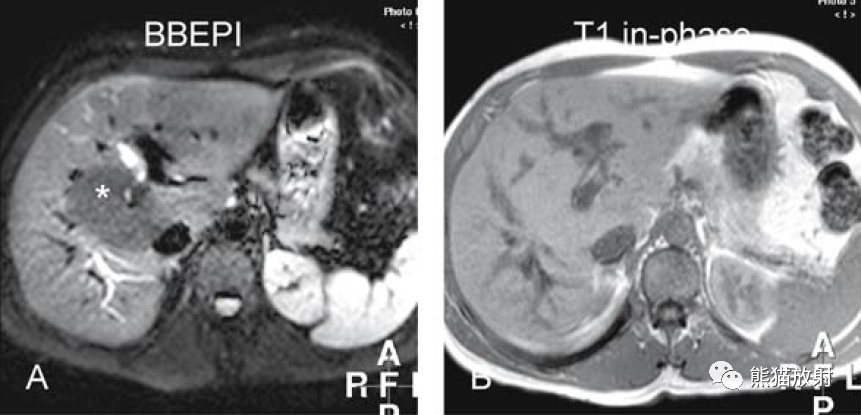
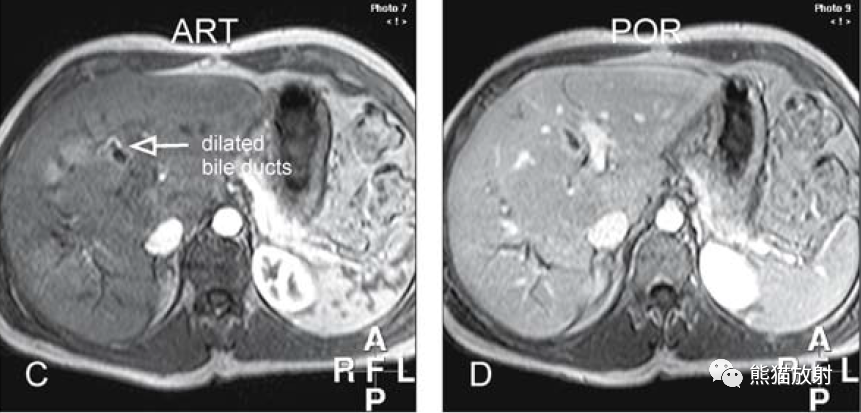
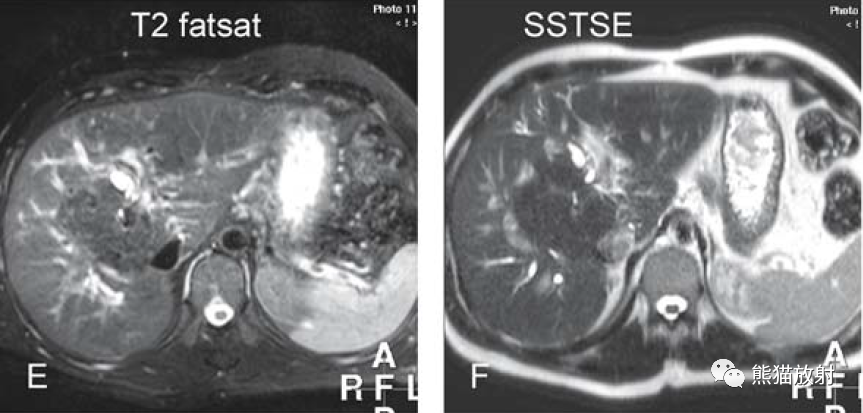
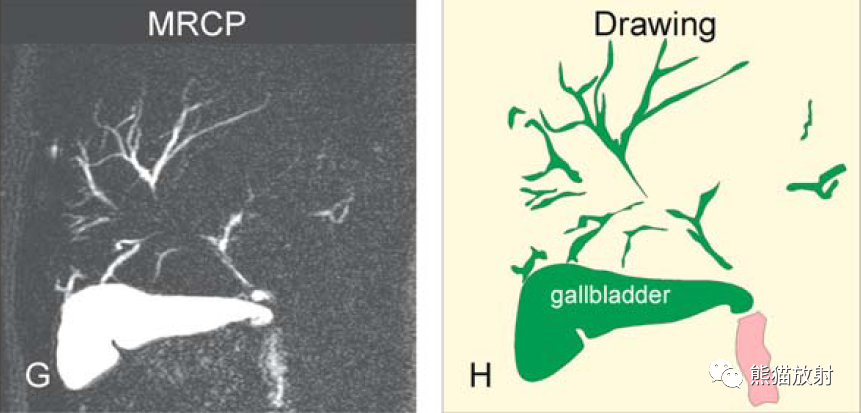
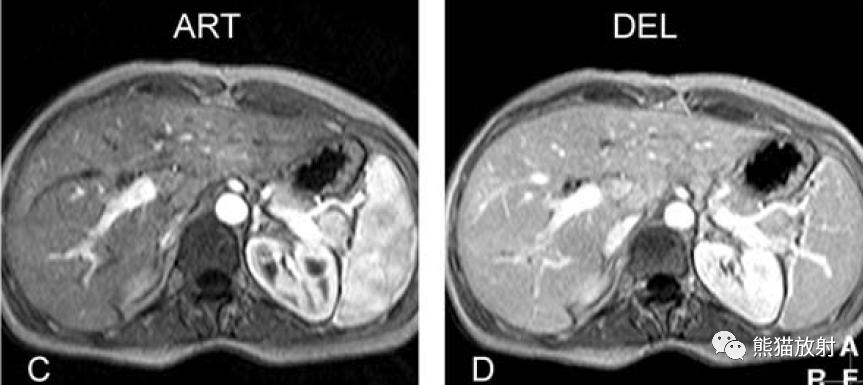
PSC。A~D图:表现如上所述。E图:T2WI-FS上扩张胆管与周围高信号血管不易区分;F图:T2WI上扩张的肝内胆管可延续至肝被膜下;G、H图:MRCP示PSC典型表现,胆囊增大提示排空受阻,胆总管狭窄所致。
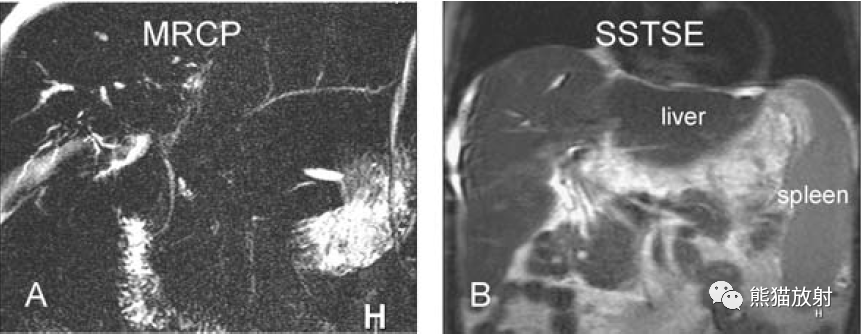
PSC(另一患者),并肝纤维化/肝硬化,脾大,反复发作的胆管炎导致节段性肝萎缩。
原发性硬化性胆管炎(PSC)的特征是慢性炎症和胆管纤维化。
小、中、大胆管的进行性和闭塞性纤维化会导致继发性胆汁性肝硬化和胆汁淤积,从而导致肝功能不全。
30%的PSC患者因胆汁淤积而发生原发性色素性结石。
MRCP对PSC中胆管的渐进性闭塞具有很高的敏感性(83–89%)和特异性(92–99%)。MRCP通常显示肝内和肝外胆管的管径变化,并有胆汁淤积的迹象(在T1WI上扩张胆管内有高信号),在T2WI上可见高信号的反应性周围淋巴结。组织学上的胆管狭窄、扩张和胆汁淤积,证实了MRI表现。

-
T2压脂:典型的胆管有长段的狭窄和扩张,延伸至肝脏外围;
-
T1同相位:胆管内的高信号归因于局部胆汁淤积(箭头);
-
增强动脉期(ART):一些扩张管周围微弱的强化提示轻度胆管炎;
-
延迟期(DEL):强化区域与正常肝实质一致。
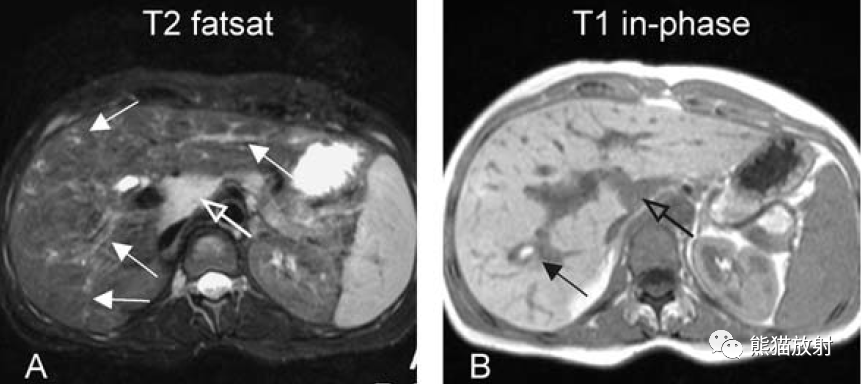
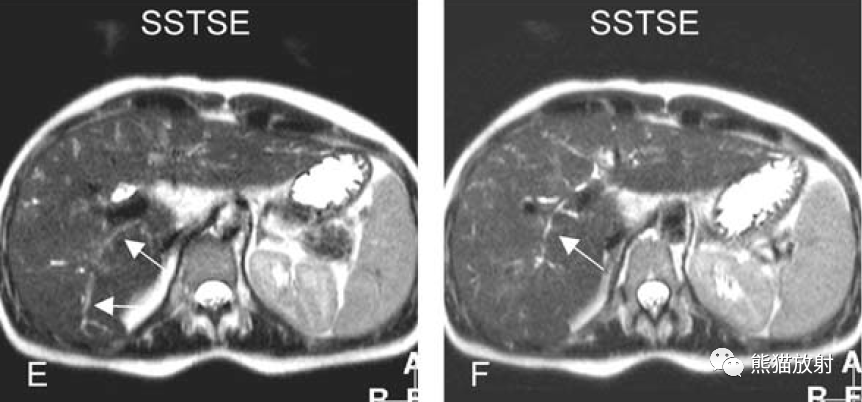
PSC。A~D图:表现如上所述。E-G图:肝内和肝外胆管异常(箭头)提示全身性疾病。H图:MRCP显示典型PSC的胆系表现,细长的肝内胆管,走行僵直,延伸至肝被膜下(箭头),肝外胆管粗细不均,管壁毛糙。
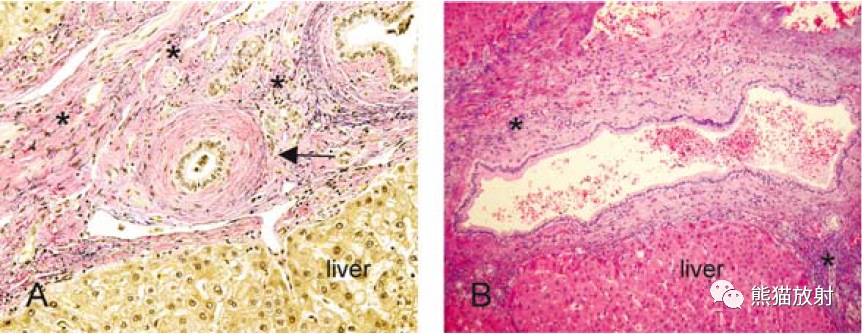
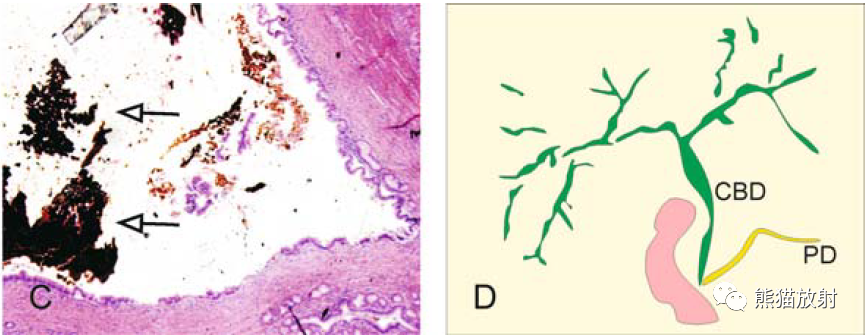
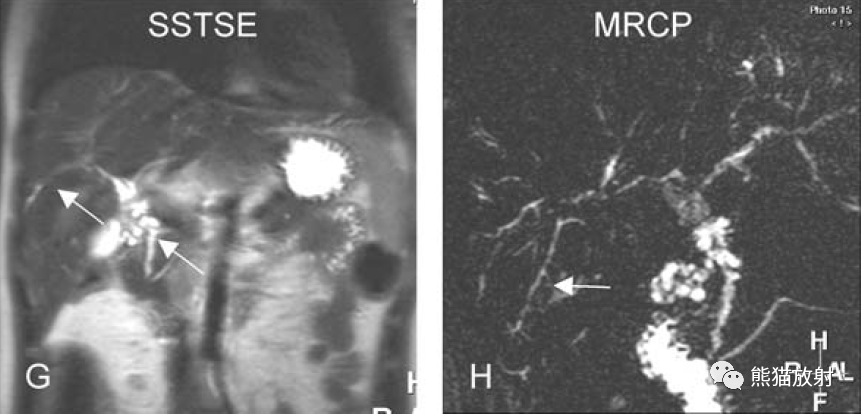
PSC。图A:镜下(HE×200)显示胆管壁增厚(硬化)和管腔狭窄(箭头)。还要注意胆汁淤积(绿色)。图B:镜下(HE×100)示胆管被纤维化和碎屑包围。图C:镜下(HE×40)示胆管扩张并胆汁淤积(箭)。图D:示意图显示PSC的典型枯树枝样外观(CBD =胆总管;PD =胰管)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#primary#
57
#PRIMA#
36
#原发性#
50
#ROS#
38
#PSC#
35
#原发性硬化性胆管炎#
43
#硬化性#
43
#cholangitis#
33
#胆管#
35